What is Endometriosis?
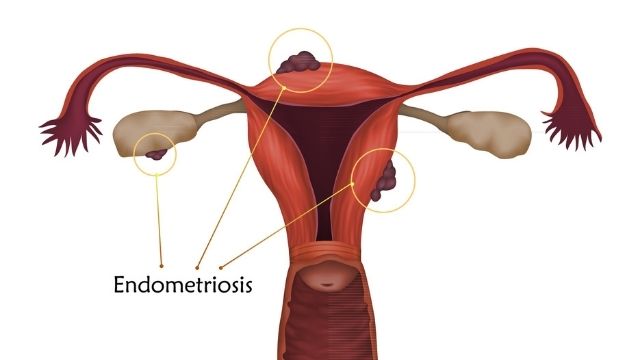
Endometriosis is a painful condition. This disease develops when the endometrial-like tissue acts as a wound, thickening and bleeding during menstruation. However, it cannot find an exit and becomes trapped, forming underlining. It develops within the uterus, while the endometrium develops outside of the uterus.
Endometriosis can develop in your fallopian tubes, ovaries, or pelvic lining. Endometriosis can exacerbate infertility in severe cases. Endometriosis can cause severe pain during menstruation.
Types of Endometriosis
There are mainly three categories of Endometriosis; it is as follows:
- Greatly infiltrating Endometriosis:
This type mainly develops in organs other than the uterus, such as the bowels or urinary bladder. It develops beneath the peritoneum. This type of Endometriosis affects one to five percent of women.
- Peritoneal lesion:
The lesion formed on the peritoneum area lines a thin lining in the pelvic region in this type of Endometriosis. This type is common in women.
- Endometrioma (ovarian injury):
These are deep red and develop deep within the ovary. It is also known as a chocolate cyst due to its deep red colour and fluid texture. They are usually incurable and have the potential to harm healthy tissue.
Symptoms of Endometriosis
The common signs that you may notice while suffering from Endometriosis are:
- More painful menstrual cramps: Pelvic pain may become more severe. It may begin several days before the period and continue afterward. You may also feel pain in your abdomen and lower back. The pain you feel during menstruation may become worse.
- Pain during intercourse: You may feel excruciating pain during or after intercourse.
- Pain during excretion: Pooping or peeing will be painful, especially during the menstrual cycle.
- Excessive bleeding: During periods, blood flow may increase. On regular days, there may be blood in your stool or urine.
- Infertility: You may be experiencing infertility issues.
- Others: You may also experience unusual tiredness, constipation, diarrhea, nausea, and other symptoms.
When to see a doctor?
If you notice any of the above symptoms in your body, you should see an endometriosis specialist right away. If you are in HYDERABAD, you can schedule a consultation with our expert Dr. ShreeTheja to begin your treatment.
It is not necessary to be in excruciating pain for the problem to be severe. Even if you have mild pain, it is possible that you have severe Endometriosis. The severity of the problem is not determined by the intensity of your pain.
Endometriosis can be confused with other conditions such as irritable bowel syndrome, an ovarian cyst, or pelvic inflammatory disease. Because these diseases share symptoms such as diarrhoea, extreme abdominal pain, and constipation. However, this does not mean you should disregard it. A doctor’s consultation can assist in preventing the serious problem.
Causes of Endometriosis
The causes of Endometriosis are not specific but might develop due to the following reason:
- Retrograde menstruation: The condition in which period blood flows back to the fallopian tube into the pelvic region rather than out of the body. Endometrial cells in the blood adhere to the walls of the pelvic organ. During the menstrual cycle, these cells multiply and thicken.
- The peritoneal cells’ lining: After transformation, the peritoneal cells behave like endometrial-like cells and line up in the inner walls of the abdomen.
- Due to embryonic cell: Estrogens convert embryonic cells into endometrial-like cells that can form lining.
- Transportation of endometrial cells: The blood vessel or lymphatic system transports endometrial cells-containing blood to other parts of the body.
- Weak immune system: If you have a weakened immune system, you may not be able to prevent the formation of endometrial-like tissue.
How to diagnose Endometriosis?
- The doctor may perform a pelvic exam to check for cysts or scars inside your uterus.
- A CT scan or an ultrasound image can tell you if you have Endometriosis.
- A laparoscopy may be performed by the doctor by cutting a small hole in your stomach and inserting a thin tube containing a camera. It allows the physician to see lesions or scar tissue.
- Following laparoscopy, the doctor may remove a small piece of tissue to examine under a microscope.
What are Endometrial cysts?
When tissue gets accumulated in the inside walls of the ovaries, they form a cyst. These are the size of lumps and can be two or more. The cysts are usually 2 inches in length; however, they can grow up to 8 inches.
These cysts can cause the following problem:
- May result in ovarian cancer
- Can make infertility treatments more difficult.
- Cause severe pelvic pain.
- Frequently reduces the likelihood of pregnancy.
- Interfere with the ovarian function.
Endometriosis stages
There are four stages of Endometriosis:
Stage 1: There are fewer lesions and no scar tissue in this stage.
Stage 2: This is the mildest stage; you have a few more lesions but no scar tissue. They form in a two-inch area of the abdomen.
Stage 3: The lesion has grown deep, containing scar tissue, and has developed in the fallopian tube and the ovaries.
Stage 4: This is the most severe stage, with numerous lesions and the ovary containing numerous large cysts. Scar tissue can be found in the fallopian tube, ovaries, uterus, and bladder.
The stage of endometriosis determines the treatment. It is always a good idea to consult the best endometriosis doctor, who will advise you on the stages and the best treatment for you.
Treatment for Endometriosis
There is no scientifically proved treatment to it; however, some medications or surgery can provide relief; they are as follows:
- Pain medicine: The doctor may prescribe pain relievers such as nonsteroidal anti-inflammatory drugs. Ibuprofen, Motrin, and Aleve are examples of such medications. These medications are extremely effective in relieving pain.
If you do not feel relieved, you can take personal measures such as taking a warm shower or performing a hot fomentation technique on your stomach. Exercise on a regular basis can also help with pain.
- Hormonal therapy: Some doctors recommend hormonal therapy to reduce the amount of oestrogen released by the body. Because oestrogen levels are reduced, there is less lesion formation, which prevents inflammation, cyst formation, and scarring.
Birth control pills, gonadotropin-releasing hormone, progestin, or danazol are examples of hormonal therapy.
- Surgery: In some cases, surgery is the only option for a woman. The affected tissue will be removed from the body during surgery. Women who have had surgery may be able to conceive again.
Surgery for Endometriosis
If you’ve tried and failed to conceive, your doctor may advise you to have surgery. If no amount of medication or hormonal therapy has helped, surgery may be an option. To remove the unwanted tissue, the doctor may use standard surgery or a laparoscope.
Endometriosis tissue removal can increase the likelihood of pregnancy. However, if you are considering a hysterectomy, this involves removing the uterus or even the ovaries, both of which are required for pregnancy.
What to expect after endometriosis surgery?
If you have had laparoscopic surgery, you will be able to recover quickly. However, if you have had a hysterectomy, you will need time to recover. You will need to take extra care of yourself, and the doctor may limit your activity.
Take your doctor’s advice on how many days you can return to your normal routine. However, recovery from a hysterectomy can take four to six weeks.
Because of the trapped gas in the abdomen, you will experience shoulder pain following laparoscopic surgery. There will be no more periods. You will enter menopause if your doctor removes your ovaries.
Endometriosis Complications
Endometriosis can cause a slew of issues in a woman’s life. As a result, some women experience depression and anxiety. Endometriosis affects about one-fourth of all women who struggle with infertility.
The resulting inflammation can harm or weaken the egg or sperm’s ability to fertilise. It can also make transporting the eggs difficult. It can, however, be treated with proper medical care.
Scar tissue can cause a blockage in the fallopian tube in some cases. Some women develop ovarian cancer or endometriosis-related cancer known as endometriosis-associated adenocarcinoma.
Endometriosis Risk Factors
There are several risk factor associated with Endometriosis, as mentioned below:
- Problem with infertility.
• Heavy flow during the menstrual cycle and last for longer days.
• Frequent menstrual cycle.
• Unusual weight loss.
• Experiencing late menopause.
• Release of hormones like estrogens in a larger quantity.
• Reproductive organ abnormalities.
Endometriosis Diet Tips
You can include the following in your diet:
- Take food containing omega-3 fats.
• Avoid eating unhealthy food containing trans-fat.
• Do not eat red meat, especially those that are processed.
• Increase the intake of fruits, whole grains, and vegetables.
• Avoid drinking caffeine and hard drinks as much as possible.
• Go for a gluten-free diet.
Endometriosis Surgery Cost
Endometriosis surgery can be intimidating. It is critical to undergo surgery in severe conditions in order to avoid future problems. In India’s major cities such asHyderabad,Mumbai, Bangalore, etc.,, the average cost of the surgery may range from Rs. 50,000 to Rs. 150,000. This amount only includes the direct price and may vary depending on a variety of factors. This number may also vary depending on which hospital you are attempting to visit.
Menstrual Problems

What are Menstrual Problems?
The menstrual cycle refers to the regular changes in the activity of the ovaries and the endometrium that allow reproduction to occur. During the menstrual cycle, women experience drastic hormonal fluctuations as well as physical discomforts such as abdominal cramps, headaches, and so on. An entire menstrual cycle typically lasts between 24 and 38 days, but this can vary from cycle to cycle and over time. The length of the cycle varies between menarche and menopause.
What are the phases of the menstrual cycle?
- If the egg has not been fertilised, the first stage of the menstruation cycle occurs, which lasts three to seven days and is more commonly known as a period because the egg has not been fertilised. Because the uterine lining, known as the endometrium, is no longer required, it degrades and is lost through the vaginal canal with some blood.
- After menstruation, the woman is most fertile during the next stage, known as ovulation. The uterine lining thickens again in preparation for a fertilised egg, and the follicle develops inside the ovary after about 14 days.
The menstrual cycle is made up of two linked and synchronised processes. The ovarian cycle is concerned with the development of ovarian follicles and ovulation, whereas the uterine or endometrial cycle is concerned with the way the functional endometrium thickens and sheds in response to ovarian activity.
Most common menstrual problem
Menstrual disorders are classified into two types: those with heavy or frequent bleeding and those with less heavy or infrequent bleeding. The most common cause of heavy or frequent bleeding is structural, most commonly in the womb. It could be a fibroid, which is a localised swelling of the womb muscles. If the fibroid pushes into the womb cavity, it can cause both irregular and heavy bleeding.
Less frequent or heavier bleeding can also indicate an underlying disorder, most commonly a hormonal disorder. When there is polycystic ovarian syndrome, this occurs naturally. This is primarily a diabetes and insulin resistance-related disease. As a result, it worsens with weight gain. The ovaries and endometrium each go through their own set of changes that are distinct but related.
When to see a doctor
If you have multiple menstrual cycles, you should see a doctor. In most cases, hormonal therapy is required to treat it. They will advise you on the best option.
Menstrual symptoms
Mensuration is the process of vaginal bleeding. As part of the menstrual cycle, the process occurs once a month. A typical menstrual cycle can last 28 days.
During this time, different women may experience a variety of symptoms. Some of them may be experiencing contractions or pain in the lower abdomen. Some women experience feverish symptoms when their period begins. Many women experience constipation prior to the start of their period. Some women may also experience puffiness or swelling in the lower abdomen.
Signs of menstruation
Different women experience different types of symptoms prior to the start of their period. The oestrogen level begins to rise at the start of the period, which causes the milk ducts in the breasts to grow.
Some of them may experience a headache as a period sign. Other menstrual symptoms include mood changes, anxiety, anger, and impatience. Some women experience difficulty sleeping as a result of menstruation. Women may develop dark patches under their eyes as a warning sign in some cases. Migraines can occur before, during, or after menstruation in some cases.
Types of menstrual problems(Disorders)
Several disorders can be faced at the time of menstrual problems. They are mentioned below.
- Heavy bleeding at the time of menstrual
- Amenorrhea or no bleeding during menstrual
- Painful menstruation or dysmenorrhea
- Premenstrual Syndrome or PMS
- Premenstrual Dysphoric Disorder or PMDD
Causes of menstrual disorder
There are several causes for which a woman can come across due to menstrual problems.
Because of a stressful life and an irregular lifestyle, any woman can develop this disorder. Anyone can use birth control pills in some cases. It can disrupt the menstrual cycle and cause problems.
This disorder can be caused by women who have polycystic ovary syndrome. Some of them are affected by pelvic inflammatory disease. This type of situation can also occur in people who have premature ovaries.
Menstrual problems complications
While you are suffering from a menstrual problem, there are several complications that you can face. Here we have mentioned some of the critical difficulties. Check the list below.
- When you have a menstrual problem, you may experience complications such as ovulation problems.
- Menstrual pain can lead to serious complications such as uterine lining issues. In most cases, this problem can also cause thyroid problems.
- People with severe disorders may develop pregnancy disorders as a result of this complication.
Diagnosing menstrual problems
Girls are expected to have a period. Things become complicated when the girl suffers from this period for an extended period of time. If you notice that your menstruation is going well, you should see a doctor. It can be difficult to pinpoint the exact cause of abnormal periods. You must correctly diagnose the problem and then take appropriate action.
Treatment for menstrual problem
Periods are one of the most common presenting symptoms for many female patients who visit the doctor on a regular basis. The treatment of the problem will be determined by the source of the pain. If you have a heavier or lighter period, you may experience a number of health problems. To avoid this situation, you should have a thorough discussion with your doctor. A gynaecologist will assist you and direct you in the right direction. You will feel better if you listen to their advice. Antibiotics can also be used to treat pelvic inflammatory disease.
Medications for menstrual disorders
Period irregularities are common, but light or heavy periods can cause serious health problems. When a woman experiences severe pain or heavy bleeding, she should consult a doctor. If the problem persists, it is advised that you seek medical attention if your menstruation lasts less than three weeks or more than one month. However, it is preferable to consult with the best gynaecologist.
It is not advisable to take any medication without first consulting a doctor. Go to the doctor’s clinic whenever you notice any unusual health issues. You can avoid this situation by doing some indoor exercises. Most doctors advise that regular exercise and a healthy diet can protect your body from harmful substances.
Gynecological Endocrine Disorders
What is Gynecological Endocrine Disorders?
Hormones are the chemical messengers in your body that are responsible for your body’s overall development. These are produced in the endocrine glands and are quite powerful as it travels around the bloodstream, and instructs as well as tissues to perform different functions. The endocrine system regulates the various hormones in the body. A hormonal imbalance can cause a variety of issues. Although there may be several causes for the hormonal imbalance, it is important to remember that the causes are dependent on the hormones as well as the affected glands.
Causes of hormonal disorders in women
Although there may be several causes for the hormonal imbalance, it is important to remember that the causes are dependent on the hormones as well as the affected glands. While some studies claim that an imbalance in one or more hormones causes imbalance, others believe that improper functioning of a few glands is to blame. Endocrine glands have special cells that store, produce, and even release hormones in your blood.
The human body is made up of various endocrine glands that regulate hormone levels. Adrenal glands, gonads, pituitary gland, hypothalamus, thyroid and parathyroid, pineal gland, and other glands are responsible for hormonal balance. Every year, many medical conditions are reported as a result of hormonal imbalance. Lifestyle habits and environmental factors can also contribute to imbalance.
Common reasons behind hormonal imbalance include extreme stress, type one and two diabetes, hypoglycemia, overactive thyroid, obesity, poor diet, birth control medications, etc. Aside from all of this, excessive exposure to toxins, pollutants, and so on can cause hormonal imbalance. Women are naturally predisposed to hormonal imbalances throughout their lives, particularly during puberty, menstruation, breastfeeding, pregnancy, and menopause.
Because women have different endocrine glands, they must deal with hormonal disorders. PCOS, early menopause, POI (primary ovarian insufficiency), and other medical conditions can cause hormonal imbalance.
Symptoms of hormonal imbalances in women
Because hormones play such an important role in a woman’s body, any imbalance will result in a plethora of signs and symptoms. However, the signs or symptoms will differ depending on which gland is not responding properly. Unexplained weight gain or loss, a hump between the shoulders, muscle weakness, muscle tenderness, excessive sweating, depression, decreased sex drive, and so on. It is critical to recognise that symptoms vary depending on a variety of factors. Hormonal imbalances can be caused by anything, from foods to lifestyle habits. If your glands do not produce enough hormones during puberty, you will experience hormonal imbalance. From irregular menstruation to poor breast tissue development and growth rate. You can go through anything.
Hormonal imbalance and pregnancy
Pregnancy is something that women yearn for their entire lives. However, if you have a hormonal imbalance, getting pregnant will be extremely difficult. It’s heartbreaking to struggle with infertility. However, there are numerous solutions; if you are having difficulty, the solutions may be even simpler in other cases. It is critical to understand that hormonal imbalance can lead to pregnancy complications.
Even if you suspect you have hormonal imbalances, you can test for them at home. You have the ability to take things in your hands. Many experts can help you understand the hormonal imbalance. There are numerous hormones coursing through your body. However, there are a few that are important when it comes to conception. The hormone FSH, or Follicle Stimulating Hormone, is required for pregnancy. Furthermore, FSH is in charge of maintaining a regular cycle as well as producing healthy eggs.
You may have heard the term LH, which stands for luteinizing hormone. Your hormone is measured using ovulation prediction kits. Luteinizing hormone tells your body to release an egg for fertilisation. AHM, or anti-Mullerian hormone, aids in the retention of immature eggs in the body. Most doctors advise taking a hormone test to determine ovarian reserve.
Complications of hormonal disorders in women
As previously stated, hormonal imbalance causes some unwelcome complications. After all, no one wants to be a slave to hormonal imbalance because it causes so many complications. Many symptoms, such as weight gain, fatigue, and itchy skin, can be attributed to hormonal imbalance. It is critical to understand that hormonal fluctuations occur at various stages of life. Women experience extreme hormonal imbalance during puberty. Some of the most common complications caused by hormonal disorders include irregular menstruation, unwanted weight gain, infertility, and so on.
Even if you plan for pregnancy, you will not be able to conceive due to infertility issues. As a result, it is best if you consult gynaecologists because they can assist you in resolving infertility issues. Not treating hormonal disorders can sometimes cause irreversible damage to your fertility system. You will eventually develop uterine or ovarian cancer.
Tests and diagnosis-
It is critical to understand that the endocrine system includes both glands and hormones. Your body has one or two systems that aid in the coordination of various bodily functions. Hormone levels are maintained by the entire endocrine system. Maintaining hormonal balance over time and in various situations is critical for survival. However, many hormonal tests have revealed that hormone levels decrease with age. You can keep your youthful vigour with hormone replacement therapy.
Aside from the endocrine system, the nervous system is in charge of regulating your body’s functions. The nervous system and the endocrine system work together to regulate various functions in your body. For example, your body’s growth and development, metabolism, and sex drive, among other things. Doctors have developed a variety of hormonal tests that aid in determining hormone levels. Diabetes, heart disease, obesity, sleep apnea, and other complications can arise as a result of hormonal imbalance. Aside from that, if any hormones in your body are either low or high, the tests can assist in determining this. Some common symptoms must be considered when making a diagnosis.For example, hirsutism, infertility, depression, etc. Thus, you can understand that testing and diagnosing hormonal imbalance is quite easy.
Treatment for hormonal imbalances
When it comes to hormonal imbalance treatments, you will come across many options. Gynecologists these days suggest taking various treatments for fixing hormonal imbalance. Listed below are a few of them.
Estrogen therapy If you are experiencing hot flushes or other uncomfortable menopausal symptoms, your doctor may recommend oestrogen therapy. You should also discuss the risks of hormone replacement therapy with your doctor.
Vaginal estrogen Vaginal dryness is a common problem that women face nowadays. Aside from that, pain during sex is a common issue. Applying oestrogen cream or taking pills can sometimes help to alleviate this problem.
Hormonal birth control If you want to keep things simple, hormonal birth control pills are effective at regulating the menstrual cycle. Birth control pills, patches, shots, IUDs, and vaginal rings are examples of common hormonal birth control pills. These pills are effective at treating acne and hirsutism.
Anti-androgen medicines Androgen is a sex hormone that is found in both men and women. Women with high androgen levels, on the other hand, experience hair loss, facial hair growth, acne, and other symptoms. Taking anti-androgen medications will aid in the resolution of the issues.
Testosterone therapy In men, low testosterone levels can lead to poor growth. Testosterone supplements, on the other hand, alleviate the symptoms of low testosterone levels. Adolescents experiencing delayed puberty can benefit from testosterone therapy, which regulates puberty levels. Injections, gel, and patches are available as therapies.
Metformin Metformin is an effective treatment for people with type 2 diabetes. In addition, women experiencing PCOS symptoms can benefit from this medication. Despite the fact that the FDA has not approved the use of metformin for PCOS,it helps in lowering androgen levels and supports ovulation.
Uterine Fibroids
Fibroids, also known as tumours that develop with fibrous connective tissue and muscle cells, are abnormal growths that can occur in a woman’s uterus. The tumours can grow to be quite large, causing severe abdominal pain and heavy bleeding during the menstrual cycle. Because fibroids are asymptomatic, they are difficult to detect. It is, however, not cancerous. According to the research, nearly 80% of women experience fibroid growth at varying rates. There are treatments available to help you find relief. Uterine myomas, Leiomyomas, Fibromas, and Myomas are all names for fibroids.
Essential facts about Fibroids:
By now, we all are aware of fibroid. But, still, there are specific vital facts that you need to know. Such as,
- Fibroids are non-cancerous tissue masses that form within the uterine wall or surface.
- Fibroids range in size. They are sometimes the size of seeds and other times the size of a watermelon.
- Fibroids can cause a variety of symptoms or none at all. Some of the most common symptoms are painful intercourse, pelvic pain, and so on.
A specific risk factor exists when developing fibroids in the uterus and pelvis. Among the risk factors are:
- The risk of becoming obese or overweight increases significantly.
- Fibroids can affect any woman at any age.
- Menopause usually occurs between the ages of 30 and 50 years.
These are the essential facts about the problem that you should be aware of.
Who gets fibroids?
Fibroids, also known as myomas or leiomyomas, are tumours. They are non-cancerous and have a very low risk of developing into cancer. It is common in women during their reproductive years, and it can grow along the cavity wall as well as into the uterus.
Many women will experience uterine fibroids at some point in their lives. Fibroids affect more than 30% of women in the United States at some point in their lives. The problem mostly affects people between the ages of 30 and 50.
Obese or overweight women are at a higher risk of developing uterine fibroids. Obesity raises oestrogen levels (a female sex hormone), and as a result, the likelihood of developing fibroids rises.
Women who have a child have a lower risk of developing fibroids. It will reduce your chances of developing fibroids if you have more than one child.
Types of Fibroids
There is a variety of Fibroids which are classified based on the location of the uterus. Hence, it is essential to know the type of fibroids. So, let us have a look below:
- Intramural fibroids
These are the most common types of fibroids in a woman’s uterus. They are most commonly seen at the uterus’s muscular cell. This fibroid grows larger and more shaped, stretching your womb.
- Subserosal Fibroids
It is also referred to as a serosa. This fibroid is most commonly found on the uterine wall. This also grows larger, making the womb appear significant on one scale.
- Pedunculated Fibroids
A pedunculated fibroid is a stem that is noticed by the growth of a subserosal tumour to provide support. It has the appearance of a thin base.
- Submucosal Fibroids
This is uncommonly formed, as far as I can tell. It usually appears in the uterus’s middle layer.
These are some of the essential types of fibroids that you should be aware of. Various factors lead to fibroid growth, such as hormones if there is any family history, or during pregnancy. Hence, it would be best if you took proper measures if you do not have a fibroid. And in case you have a fibroid, you must undergo appropriate treatment so that it does not lead to something severe.
Nowadays, there are various diagnostic measures with the help of which you can quickly identify fibroid and undergo the necessary treatment that is needed.
Causes for Uterine Fibroids to Grow
It isn’t easy to find out the actual cause of forming fibroids in the uterus. Gynecologists have failed to explain why fibroids increase and shrink in size. Let’s check out some of the major factors for which the problem appears.
- Hormone Factor
During each menstrual cycle, oestrogen and progesterone stimulate the development of the uterine lining in preparation for pregnancy and promote the growth of fibroids.
- Genetic Changes
According to some researchers, fibroids may be hereditary because many fibroids contain gene changes that differ from those found in normal uterine muscle cells. There is, however, no conclusive evidence of this.
- Growth Factors
Some substances, such as insulin-like growth factors, aid in tissue maintenance and may influence fibroids’ growth.
- Pregnancy
You might be wondering about the connection between pregnancy and fibroids. Fibroids do not usually interfere with getting pregnant. However, fibroids, particularly submucosal fibroids, may be a cause of infertility or pregnancy loss. and a large intramural fibroid of more than 4 cm can interfere with fertility.
Risks of uterine fibroids during pregnancy
It may also raise the risk of certain pregnancy complications such as abruption, fetal growth restriction of the baby, preterm delivery, etc. Let’s check out the dangers of uterine fibroids during pregnancy.
- Restrict Fetal Growth:
When the size of the fibroids increases, the length of the womb decreases, preventing the embryo from growing.
- Placental Abruption:
Placental abruption occurs when a fibroid blocks the uterine wall. It may deplete nutrients and oxygen, both of which are essential components of your body.
- Preterm Delivery:
You will experience pain as the size of the fibroids increases. This discomfort causes uterine contractions. It results in earlier delivery.
- Breach Position:
Because of the abnormal shape of the cavity, the baby may not be able to align for a standard delivery.
- Cesarean Delivery:
According to the researchers, women who have fibroids are six to seven times more likely than those who do not have this type of issue in their bodies to require a caesarean delivery.
- Miscarriage:
The chances of miscarriage are doubled in women who have suffering from this problem.
Symptoms of Fibroids
Fibroid symptoms can differ. Fibroid symptoms vary depending on the size, location, and number of tumours. Because uterine fibroids do not cause symptoms, women may be unaware they have them. During a pelvic examination or prenatal ultrasound, a doctor may discover uterine fibroids by chance. However, the following are the most common symptoms in symptomatic women:
- During the menstrual cycle, there is a lot of bleeding.
- More than seven days, which is longer than the average menstrual period.
- There may be a bloated sensation in the lower abdomen.
- In the pelvic region, there would be pressure or even pain.
- Constipation may be the cause of fibroids in a woman.
- There may be a stronger desire to urinate frequently.
- You may experience pain during sex.
- Difficulty in conceiving is infertility.
- The reproductive issue includes miscarriage, preterm delivery, etc.
We would like to emphasise that having any of these symptoms does not necessarily indicate that you have fibroids. These are general symptoms that could be caused by a variety of factors. As a result, it is recommended that if you notice any of these symptoms, you consult a gynaecologist, who will perform the necessary tests to confirm the diagnosis.
How are fibroids diagnosed?
The majority of the time, ultrasound is used to diagnose fibroids. They can then be interpreted in terms of fertility by a saline infusion sonogram or a hysterosalpingogram (HSG).
The doctor performs some necessary tests to determine whether you have fibroids or not, such as hysterosalpingography, blood tests, ultrasound tests, and so on.
Treatment for uterine fibroids
Treatment is only advised if there are any symptoms. If you have symptoms, consult your doctor, who will recommend the best treatment plan based on the size and location of the fibroid.
- If the fibroid is well away from the cavity, not changing the shape of the cavity, and not causing you any other symptoms, there is no reason to have it removed. So, if the fibroid is changing the shape of the cavity or causing some of the other symptoms, doctors will usually advise you to have it removed.
- Some doctors advise waiting and watching to determine whether or not treatment is necessary. Some people recommend taking medications to regulate your menstrual cycle or to treat symptoms like heavy menstrual bleeding and pelvic pressure. Medication will aid in the reduction of fibroids in size. Various medications are available.
- Gonadotropin-releasing hormone (Gn-RH) agonists are one of them. They treat fibroids by increasing oestrogen and progesterone production, putting you into a temporary postmenopausal state. As a result, menstruation ceases, fibroids shrink, and anaemia frequently improves with patience.
- Another important medical treatment is a progestin-releasing IUD, which can stop heavy bleeding caused by fibroids.
- Hysterectomy is another treatment option for fibroids. This is the removal of the uterus and a permanent solution to the prevention of fibroids, which is usually indicated if the patient’s family is complete.
- The latest technology is used in a non-invasive procedure to destroy the fibroids using an ultrasound transducer. Magnetic Resonance-guided Focused Ultrasonography is another name for it. The fibroid tissues are routed using ultrasound rays in this procedure.
- Uterine artery embolisation is another minimally invasive procedure for removing fibroids.
Hence, these are the different treatment options available depending on the number of fibroids, size of the fibroids, symptoms of the patient, and age group of the patient.
Medical treatment for fibroids
Other medications are also available to reduce the size of the fibroids as well as bleeding loss. A doctor may advise a Myomectomy, which is a procedure to remove the fibroids. Depending on the size and location of the fibroid, this procedure can be performed laparoscopically or through open surgery.
Surgery for Fibroids
Typically, fibroids are removed in one of two ways. You can have them removed surgically, either laparoscopically or openly, by making an incision in your belly and removing the fibroids. During the procedure, the doctor inserted a small camera into the uterus and examined it. The entire fibroid is visible. In this case, the recovery time is even shorter.
Cost of uterine fibroid surgery
The cost of uterine fibroid surgery is dependent on the type of surgery required. For example, if you want to do a Hysterectomy, it will cost around 1,85,000 in Indian rupees. This is the latest technology to remove a fibroid. Another surgery such as Myomectomy, Endometrial Ablation will cost up to 1,65,000 to 1,70,000.
Cosmetic Gynaecology

How does cosmetic gynecology work?
Cosmetic gynecology also helps to improve the labia and vagina’s appearance and function. It might also help make sexual activities better. Cosmetic gynecology also gives the body’s genitalia a more youthful and appealing appearance. The vagina’s appearance has changed over time due to events like pregnancy and birth. Additionally, it alters its response to the stimulus. Corrective gynecology can assist with reestablishing this. Women can gain happiness and self-confidence through this procedure.
Who really requires cosmetic gynecology?
A woman who is unhappy with the appearance of her vaginal area is a good candidate for cosmetic surgery. This is for those who are dissatisfied with the way she feels or works in her vaginal area.
If you are aware of the procedures’ risks, you might be a good candidate. Additionally, when you are in good health and have reasonable expectations regarding this procedure. If you want to have the procedure but are concerned about your health, you should talk to your gynecologist.
Diabetes, high blood pressure, depression, bleeding disorders, and heart disease are among the health problems. In addition, you must be aware that you are the ideal candidate for this procedure if you are overweight or obese and addicted to alcohol or smoking. Before considering this treatment, strict abstinence from addictions must be observed.
Cosmetic gynecology can be chosen by a woman for a variety of reasons. For example:
The gift to a partner for religious reasons to boost self-esteem to improve the appearance of the lips or labia to boost sexual desire and performance to improve treatment options from which you can benefit
Non-surgery
Surgery
Preparation
reparation You must first physically and mentally prepare yourself for the cosmetic gynecology procedure. To assist you with getting ready better for this treatment, here are a portion of the tips are :
Your body weight must be proportional to your height. Maintain a healthy BMI You shouldn’t have diabetes or heart disease. For the best advice, tell your doctor everything you’ve ever been through.
Follow severe limitations on Compulsion for the expressed term as suggested by your PCP.
You ought not be an enemy of misery medicine. Attempt to have great mental prosperity.
Treatment Options For Cosmetic Gynaecology
Types of Procedures in cosmetic gynecology
There are five main types of cosmetic gynecology. You must be well aware of the different types of gynecology before you opt for one.
Vaginoplasty
This procedure helps to tighten the vagina. It also helps in rejuvenating the vagina for sexual satisfaction.
Monsplasty
A monsplasty is a procedure designed to reduce bulging of the mons. It helps to tighten, lift, and shape-up the bikini bridge, the pubis. This is because it becomes prominent while wearing different types of outfits.
Hymenoplasty
Hymenoplasty is a cosmetic surgery for women who may wish to repair or reconstruct their hymen. This procedure helps to create an entire hymen that might be broken due to cycling or horse-riding.
Hoodectomy
A simple procedure in which the clitoral hood is shortened. It improves the aesthetic appearance as well as sexual function in women.
Labiaplasty
In this procedure, the size of the lips of the vagina is reduced, and also the appearance of the inner labia is improved. You can read more about this labiaplasty here.
cost of cosmetic gynecology
Well, the cost is the most significant aspect of everything. Before beginning treatment, you must determine whether you can afford it. In India, the techniques would in the middle between Rs. 2,00,000 to Rs. 3,00,000. However, the entire procedure—chondroplasty, labioplasty, perineoplasty, hymenoplasty, labia majora augmentation, and labia majora reduction—would set you back approximately Rs. 10 lakhs.
Result of cosmetic gynecology surgery
Cosmetic gynecology surgery rejuvenates the genitals while simultaneously enhancing sexual activity. It makes the body stylishly satisfying and shows up a lot more youthful. People who wish to go through this strategy gain self-assurance. The quality of life can be improved by this procedure. It also makes you happier and gives you more energy.
Vaginal Reconstruction

What exactly is vulvar rejuvenation?
The vagina can change with age and childbirth, and some women want to get it back. After having a vaginectomy (surgery to remove the vagina), a woman can undergo vaginal reconstruction, which is the surgical procedure of creating an artificial vagina. After having surgery to remove your vagina, you must ask your doctor if a vaginal reconstruction is possible. One of the goals of vaginal reconstruction is to allow for sexual activity in the vagina. A plastic surgeon uses muscle and skin from other parts of the body for the reconstruction during this procedure.
Everything You Need to Know About Vaginal Reconstruction
Ideal candidate for vaginal rejuvenation
Everyone is not an excellent candidate for vaginal rejuvenation treatments. The ideal patient for vaginal rejuvenation is a woman who has had multiple births and has less sensation during their sexual encounters.
A decent competitor is likewise the person who has irritation or torment while sexual exercises, riding a bicycle, or horseback riding. Women whose uterus has changed as a result of childbirth can benefit most from this procedure.
Why women do vaginal surgery?
Any woman’s uro-vaginal regions can be affected by accidents or birth defects. The sensation of the vagina can be restored through a variety of treatments, including non-surgical and surgical procedures. The following are some of the reasons why vaginal surgery is necessary:
- to fix the defects that were born.
- to rebuild the cancer-afflicted reproductive system and urinary tract. Radiation therapy and organ transplants are common treatments for cancer patients.
- to treat vaginal prolapsed women.
- to rehabilitate and rejuvenate the genitals damaged by accident and rape.
Vaginal rejuvenation before and after
The pelvic and vaginal regions may be damaged or have excessive skin prior to the vaginal rejuvenation. The vaginal canal may become wider and the opening may become larger, as well, according to the doctor. There will be decreased sexual joy.
The vaginal canal will become narrower and the openings will become smaller following the vaginal rejuvenation procedure. The labia will be reduced and reshaped, but the excess skin around the vaginal canal will be removed.
What are the risks of a vaginoplasty?
Vaginoplasty is associated with two kinds of dangers. The first is a general risk, and the second is a particular risk.
General risks Infections, bleeding, and anesthetic-related accidents are some of the general risks associated with the surgery. If the patient is in good health before the surgery, there are very few risks.
Specific risks Vault prolapse, vaginal fistula, and uterovaginal are just a few of the specific risks associated with the surgeries. It depends on whether the individual has diverted colitis as well as colitis that affects the uterus.
How to Get Ready for a Vaginal Rejuvenation Surgery Your doctor will tell you how to get ready for the surgery. Before the surgery, you will be asked to stop drinking alcohol, smoking, taking steroids, or taking any other medication. You will quickly recover if you follow these guidelines.
What are the potential complications?
Complications related to vaginal reconstructions are similar to that of any other surgery which involves a general anesthetic. Some of the common complications are:
- Infection
- Pelvic pain
- Neurologic injury
- Bleeding
- Bladder injury
Treatment Options For Cosmetic Gynaecology
Procedure of Vaginal Rejuvenation
Vaginoplasty is associated with two kinds of dangers. The first is a general risk, and the second is a particular risk.
General risks Infections, bleeding, and anesthetic-related accidents are some of the general risks associated with the surgery. If the patient is in good health before the surgery, there are very few risks.
Specific risks Vault prolapse, vaginal fistula, and uterovaginal are just a few of the specific risks associated with the surgeries. It depends on whether the individual has diverted colitis as well as colitis that affects the uterus.
How to Get Ready for a Vaginal Rejuvenation Surgery Your doctor will tell you how to get ready for the surgery. Before the surgery, you will be asked to stop drinking alcohol, smoking, taking steroids, or taking any other medication. You will quickly recover if you follow these guidelines.
Post-Treatment Aftercare
There is a difference between the post-treatment care for surgical and non-surgical procedures.
Patients begin to recover from surgical vaginal rejuvenation six weeks after the procedure. Patients will be instructed to walk as soon as the anesthesia wears off following the surgery. The surgeons will first advise the patient to apply ice packs to reduce the swelling, pain, and bruising.
After surgery, painkillers will also be prescribed to alleviate discomfort. The following 72 hours after the surgery, the doctors will recommend that you limit your exercise and wear loose cotton clothes. Patients will be told to stay away from sex, swimming, or involving a bath for the following a month and a half after the medical procedure. Horseback riding, four-wheeling, and motorcycle riding must all be avoided.
The recovery period for non-surgical vaginal rejuvenation, such as filler augmentations or laser rejuvenation, is significantly shorter and painless. After the non-surgical procedure, sexual activity is prohibited for about a week after the surgery.
Recovery after vaginal rejuvenation
After the vaginal rejuvenation procedure, there will be soreness, swelling, and bruising. It will take about a week or two for them to recover. After a few days of the surgery, patients will be able to walk comfortably. You will get the final result after a couple of months of the surgery. Also, you will be able to resume sexual activity after 4-6 weeks of the surgery.
Benefits of vaginal rejuvenation procedures
The six benefits of vaginal rejuvenation procedures :
- Enhance your sexual satisfaction
- Customize your individual needs
- Re-impose tightness to the vaginal area
- Your partner’s sexual appearance will be improved
- Urinary inconstancy will be improved.
Vaginal Rejuvenation cost
The procedure itself will cost anywhere from Rs. 30,000 to Rs. in India, 50,000 Medication will not be included in the cost.
Hymenoplasty

What is Hymenoplasty Medical procedure?
At the point when the messed up hymen is reestablished through a medical procedure, it is known as hymenoplasty or hymnography. This corrective fix of the hymen is otherwise called revirginization. You shouldn’t be worried about the surgery because the doctors will give you local anesthesia to ease your pain. To learn more about the procedure, you must first be familiar with the hymen’s specifics.
Everything You Need to Know About Hymenoplasty Surgery
What is the hymen?
The tissue that covers the vaginal opening is called the hymen. It is found in the vagina. It usually develops during the carrier’s fourth month of pregnancy, when the female baby is still in the womb. A hymen might tear or separate. However, the harm might not last forever. The damage can be treated in a few different ways.
The purpose of hymenoplasty
Because it is only a cosmetic fix, this surgery may not be necessary. However, you may need to get this treatment because of some serious issues. The reasons could be anything from physical to mental. The following are some of the discussions surrounding this.
Blocked Hymen:
Because the membrane is blocked, this could be a serious issue. This, in turn, prevents blood flow, which would impede menstrual flow. In order to facilitate flow, a small hole is cut in the hymen.
The septate hymen is a type of hymen with an intricate structure. When this occurs, the hymenal tissue splits into rope-like formations, resulting in a complex structure. As a result, the hymen may become extremely thick. A hymectomy is carried out so that any issues caused by the thickness can be avoided.
In order to treat accidental ruptures, the hymen may frequently be damaged unintentionally. For the purpose of restoring the hymen, you can opt for hymenoplasty if you consider it unacceptable.
Flaccidity in the vaginal muscles can occur after childbirth or with age. Muscle tightening This can be relieved by hymenoplasty.
You can opt for this procedure to achieve psychological contentment. This is the simplest solution because the lack of hymen may make you feel uneasy or worried.
Who would be the best candidate?
Motives could be sexual or not sexual. You might be the best contender for the medical procedure on the off chance that you don’t have the hymen tissue or need to supplant it. Some unmarried women want to demonstrate that their hymen has been intact, so they choose
surgery if they see any evidence to the contrary. Typically, women who have already given birth choose this muscle-tightening treatment. Or then again, young ladies who have experienced undesirable tears decide to fix it.
Hymenoplasty procedure
Using local anesthesia, this is a straightforward procedure. In it, the specific tissue is sewed so that there stays a little opening as it were. The tissues or excess skin are gently and precisely cut off.
It could happen that there isn’t sufficient skin or the hymen is none – existent. The doctor then uses some of the skin from the vagina or synthetic tissue to make one. The doctor will make arrangements for your vaginal flap or artificial blood supply in such cases.
Preparing for hymen repair
Preparing for a hymenoplasty This might scare you, but you shouldn’t be afraid of it. One of the safest and easiest procedures is this one. Feel free to talk about it with your doctor so that you can both learn about the requirements. You ought to go to clinics that treat you with kindness and compassion. The most important thing is to feel at ease and have faith in your doctor. Choose the same if you prefer female nurses and doctors for such treatment.
New surgical technique for hymenoplasty
A new surgical method for hymenoplasty is available if you are undergoing surgery to alleviate the pain of your first sexual encounter. It’s called “superhymenoplasty.” In it, an artificial super-hymen is made so that there is more bleeding after the first sexual act. Additionally, general anesthesia is required, but the doctor inserts two layers into the vagina. Under the urethral orifice, torn pieces of the hymen are inserted during the procedure.
Although the procedure ensures success, this may cause some minor discomfort. The doctors say to clean the area with warm water and use an ointment that works for your skin after the surgery. This accelerates healing. This is a fake method for reestablishing your hymen, thus it in no way hurts to the vagina.
Treatment Options For Cosmetic Gynaecology
The success rate of hymenoplasty
As previously stated, this surgery is simple. However, you should be careful to follow your gynecologist’s instructions throughout the treatment and after it. It has a 98% success rate.
Hymen restoration advantage
- It will help you to have normal sexual intercourse with minimal or moderate bleeding.
- The damage caused unintentionally gets repaired.
- It can make you feel better. As a woman, you might be conscious of your body and even small harm can bother you. With this surgery, you can gain back the confidence.
Side effects and Complications after hymen restoration
Side effects and complications following hymenoplasty This is probably the only surgery that comes with concerns about risks and complications. There are no significant assemblages included. However, a stricture-related issue may arise from time to time. The vaginal opening may narrow in such a situation, making the subsequent act of sexual activity challenging.
Pain, bruising, numbness, swelling, and bleeding are some additional side effects. However, if you strictly follow the directions, you can easily treat them all.
Hymenoplasty recuperation
You can recuperate rapidly in the event that you take a rest for not many days. To fully recover, it takes between seven and ten days. After two to three days, you can resume work, but you must first avoid doing heavy work or exercise.
It’s important to remember that you can start having sexual relations after eight weeks. It will take some time for it to heal completely.
Long-term benefits are the goal of this treatment. It is effective for a considerable amount of time.
Hymenoplasty cost
The expense of the hymen fix is substantially less contrasted with other weighty medical procedures. It costs at least twenty thousand dollars and maximum fifty thousand dollars. The type of treatment provided before and after the surgery influences the price. Since this is cosmetic surgery, it’s a good idea to choose a better treatment option, even if it costs more. Your comfort and well-being ought to come first.
A novel approach to self-care is hymenoplasty. If you really care about the little things in your body, you should think about it. It’s a way to treat yourself and your body well.
Labial reconstruction

What exactly is labiaplasty?
Labiality has benefits for both appearance and function. It assists with eliminating the abundance skin in the labia, which causes disturbance by exciting bends in the road. Additionally, it aids in restoring youthful appearance after aging and childbirth. Some women who have larger labia also have trouble wearing cotton clothes. Ladies choose to go through Labiaplasty to lessen the size of the labia minora. It can stop pain when you exercise, have sex, or do physical activities. Additionally, this procedure removes some areas with lumps, bumps, or other abnormal tissue.
Everything You Need to Know About Labiaplasty
Labiaplasty procedure
During labiaplasty, either a laser or a scalpel is used to cut the excess labia tissue. Sedation and local or general anesthesia are both options for this procedure. Dissolvable, fine stitches complete the closure.
Local anesthesia is all that is required for labiaplasty. Whether the patient requires general anesthesia or not is up to them. For some patients, an oral sedative may even be necessary to ensure maximum comfort during the procedure.
There are two most famous techniques for labiaplasty – wedge or trim. A woman who wishes to remove a piece of tissue in the shape of a pie and also advances the edges of the tissue together is in need of the wedge method.
It likewise assists with fixing and psychologically the labia. The trim method, on the other hand, gets rid of any extra tissue from the labia. Labiaplasty is combined with other procedures like vaginoplasty, perineoplasty, and clitoral blood reduction.
Risks associated with Labiaplasty
There are minor complications patients undergoing the procedure may face. Here is the list of a few:
- Numbness
- Chronic dryness
- Painful vaginal sex due to scarring
- Vulvar sensitivity decreases
- Hematoma
- Infections
In case you experience any complications after Labiaplasty, then you should consult your surgeon or doctor who has performed the surgery.
Treatment Options For Cosmetic Gynaecology
Timeline for libiality recovery A woman typically needs between two and four weeks to resume her fitness routines and active lifestyle. However, the patient’s overall health is the primary factor. In most cases, it takes six to eight weeks before the scars can be used again.
What should surgery entail?
The labia’s condition prior to the procedure is significantly different from its condition following surgery. Before the medical procedure, the internal labia are either huge than the external labia or the other way around. Doctors reshape the labia and any excess tissue following a labiaplasty.
What to expect from surgery?
A labiaplasty patient can anticipate some minor bruising, swelling, or discomfort immediately following the procedure. After a few days of treatment, the majority of patients resume their normal lives. Each person’s recovery from surgery is different.
You will need to resist yourself for at least six to eight weeks following the surgery.
Cost of labiaplasty
The cost of a labiaplasty in India varies depending on the location and. The cost of the surgery is Rs. 30,000 to Rs. 60,000.
Perineal Reconstruction

What is Perineal Remaking?
The process of rebuilding damaged or deformed tissue between the anus and genitals is known as peritoneal reconstruction. This procedure also aims to correct perineal descent. In order to raise the functional vaginal introitus. The stress pressures are lessened by the restored pelvic outlet. When the anticipated defect is substantial and cannot be closed with simple sutures, peritoneal reconstruction is recommended. Consequently, it is carried out to repair flaws and restore perineal function. After this medical procedure, there are no imperfections, and there is the reclamation of perineal capabilities. It might likewise incorporate penile or vaginal remaking.
Everything You Need to Know About Perineal Reconstruction
Why is perineal reconstruction done?
Anus repositioning surgery is performed as part of peritoneal reconstruction. This procedure also aims to correct perineal descent. In order to raise the functional vaginal introitus. The reestablished pelvic outlet helps in easing the pressure pressures too.
Perineal reconstruction procedure
When there is a significant defect that cannot be fixed with stitches, doctors recommend this procedure. After this medical procedure, there are no imperfections, and there is the reclamation of perineal capabilities. This surgery also includes penal reconstruction or a vaginal one.
Congenital and acquired deformities, as well as restoration, are the primary indications for this procedure. Following surgery for cancer of the urinary and genital tract, doctors recommend this procedure. In addition, the surgeons begin by evaluating the various body states.
Nutritional status, the nature and severity of perineal wounds, blood parameters, defects, and the perineal’s function are a few examples. One of the traumatic procedures that doctors evaluate through this procedure is cancer ablation. Based on the evaluation, the surgeons determine whether a particular flap is required.
In reconstructive surgery, what are flaps?
The flap is a type of tissue that is lifted from the donor site to the defect site. Additionally, the specialists play out this with a flawless stock of blood. Some types of flaps are:
Muscle flaps: These only contain muscle tissue that fills in holes and restores functionality. It might require a cover for which skin will be used.
Cutaneous flaps: These flaps contain not only the full thickness of the skin but also the superficial fascia. These folds are great for little imperfections.
Bone flaps: These flaps are ideal for bony defects and contain bone tissue.
Fascia-cutaneous flaps consist of deep fascia, subcutaneous tissue, and a greater supply of blood. They also contain the entire thickness of the skin. It can also cover up larger flaws.
Fascia-cutaneous flaps are supplemented by musculocutaneous or myocutaneous flaps, which contain an additional layer of muscle. Additionally, it repairs deeper flaws and restores function.
Additionally, many of these body parts make excellent flaps for the perineal reconstruction process. Additionally, the evaluation of the defect aids in the selection of the flaps.
The following are the flap options:
The most frequently used Gracilis myocutaneous flaps are those in the abdomen, thighs, groin, gluteal (buttock) flaps, rectus femoris flaps, and perforator flaps.
Treatment Options For Cosmetic Gynaecology
Risk & Complications of perineal reconstruction
Risks with perineal reconstruction include:
- Local wound problems such as infection, pain, delayed healing, bleeding.
- Scarring issues such as discolouration, itching, sensitivity, the width of the scar
- Ischemia, which is the loss of tissue oxygen of the skin resulting in partial or delayed healing. Sometimes there is also a complete loss of skin.
- Temporary palsy of the largest nerve of the body. It runs from the lower back to the toes
Surgeons also ask to avoid this surgery to people suffering from the vascular disease in the lower limbs. It is because this may cause complications like:
- Pain
- Reduced sensation of touch
- Temporary weakness which lasts for an average of six months
- Tingling
- Poor reaction to anaesthesia as well
- Running, walking, and sports may have interfered with persistent weakness simultaneously
Perineal reconstruction recovery time
The patient’s condition also affects how long it takes for them to recover. Additionally, swelling and bruising following surgery last for a week or two. After five to seven days after surgery, patients can also walk normally.
After four to six weeks after surgery, patients are able to resume sexual activity and exercise. Some of the time patients may likewise feel drained and frail in the initial a month and a half. Additionally, doctors advise regular follow-up to monitor healing.
Perineal reconstruction Cost
The cost of reconstructing the perineum ranges from Rs. 2,00,000 to Rs.3,00,000.
However, there is no pain during the peritoneal reconstruction procedure. Albeit postoperative torment relies on the resistance of the patient. The surgeons also recommend regular follow-up to monitor the healing.
Urogynecology

What exactly is urology?
The sub-specialty of gynecology is-urogynecology. It is also known as Female Pelvic Medicine & Reconstructive Surgery in many countries. Clinical issues, for example, brokenness of the bladder and pelvic floor are overseen by a urogynecologist. Gynecologists or urogyns are also doctors who receive special training to treat and diagnose women with pelvic floor disorders. On the off chance that you are encountering matters connected with pelvic organs like uterine prolapse, overactive bladder, inside incontinence, urinary incontinence, and other disappointing pelvic issues, you might track down help by visiting a Urogynecologists.
Who are urogynecologists?
Urogynecologists or urogyns are also doctors who receive special treatment to treat and diagnose women with pelvic floor disorders. They complete a residency or clinical school in Urology or Gynecology or Obstetrics.
Urogynecologists are experts who have extra preparation and experience to treat the circumstances that influence the female pelvic organs. The connective tissue and muscles that support the female pelvic organs may also be affected by these conditions.
Urogynecologists do not all complete a formal fellowship. It primarily addresses non-cancerous conditions’ surgical and non-surgical treatments. Urogynecologists commonly treat the following issues:
- Pelvic organ prolapse
- Urinary incontinence or spillage
- Overactive bladder
What is the job of a urogynecologist?
Subsequent to finishing the examinations and getting a degree in gynecology, the hopeful competitors embrace a cooperation. At the very least, it lasts three years. In addition, procedures for treating incontinence, restoring and reconstructing the pelvic floor, and other issues relating to the pelvic organs are carried out.
Urogynecologists are women-only specialists. Different states of the pelvic organs alongside the encompassing muscles and tissues are seeking finding and treatment by a urogynecologist. The urogynecologist also treats pelvic organ prolapse and incontinence.
One in four women suffers from pelvic health issues like:
Pelvic organ prolapsed-Loss of the typical help of the vagina causes the dropping of the pelvic organs-pelvic organ prolapse.
Fecal incontinence, bowel leakage, and constipation are all examples of bowel control disorders, which include urinary incontinence.
Leakage is the cause of an overactive bladder’s sudden urge to urinate. The bladder spasms are to blame for this.
What kind of services does a urogynecologist provide?
When you first see a urogynecologist, they will inquire about your life experiences. Contingent upon the idea of the issue, an actual test will likewise occur. The urogynecologist will be able to better comprehend your issue with physical examinations. They will also provide you with the best treatment option.
When would it be a good idea for you to see a urogynecologist?
In the event that you are encountering matters connected with pelvic organs like uterine prolapse, overactive bladder, entrail incontinence, urinary incontinence, and other baffling pelvic issues, you might track down alleviation by visiting a specialist in this field.
Urogynecologists are specialists who treat the female pelvic organs and the pelvic floor, for example,
Muscles, ligaments, nerves, and connective tissue that control and support the rectum, bladder, uterus, and vagina.
Why do women require a urologist?
A few ladies might need to see urogynecologist since they are gynecologist with unique preparation. They treat bladder control issues as well as a variety of other conditions involving the female reproductive system and urinary tract, such as:
Urine leaks include bloody urine, sudden and frequent urges to urinate, pain in the sides or back, and a burning sensation while urinating. These symptoms often prompt women to visit a gynecologist. The previously mentioned side effects can be a justification for:
- Urinary parcel contaminations
- Fallen bladder
- Bladder control issues
- Urinary stones
- Agonizing bladder condition
- Disease
Prolapse

What is a prolapse?
There is a bulge that causes the organ to fall down when the supporting tissues that cover a part of the body weaken or stretch. Prolapse refers to the organ’s deviation from its original position. There are a few sorts of prolapse, in particular,
- Pelvic Prolapse
- Rectal Prolapse
What is prolapse of the pelvic organ?
When the organs that make up the cover or floor of the pelvic area drop down, this is called pelvic organ prolapse. This affects the majority of women. The pelvic organs are held in place by the muscles that surround them, but if there are problems, these muscles may flex and stretch. The rectum, vagina, and uterus are all part of the pelvis. One or more of these organs might stop functioning properly if there is a problem with the pelvic floor. Prolapsed pelvic organs, urinary inconsistency, and anal issues are some of the effects of a pelvic floor disorder.
Uterine prolapse, Urethrocele, Vaginal prolapse, Cystocele, Enterocele, and Rectocele are the names given to the condition in which the organs of the pelvis fall into or leave the anus or vaginal canal.
- Uterine prolapse
- Urethrocele
- Vaginal prolapse
- Cystocele
- Enterocele
- Rectocele
Symptoms of pelvic prolapse
Symptoms of pelvic prolapse It is difficult to identify any particular symptom. The affected organ is the source of the symptoms, which are not universal. You might spot the possible signs if you are extremely careful.
Constipation, pain during sexual activity, lower back pain, issues with urination, such as blood clotting or spotting during menstruation, and lower back pain are all symptoms of constipation.
Cause of pelvic organ prolapse
This mostly happens when you put more pressure on your abdomen or midsection of your body. There are a few known causes, such as hysterectomy, which is the surgical removal of the uterus.
- Disease in pelvic organ-that causes steady aggravation in the stomach region.
- Obesity can be one of the main reasons for your body flexing and stretching, which can lead to fat formation in your pelvis.
- Long haul issues connected with Hacking that can come down on your lower midsection prompting relaxing of the muscles.
- Constipation that lasts for a long time and is caused by weaker tissues connecting the organs Giving birth at a young age because the body parts aren’t ready.
Pay a visit to doctor
If you notice any of these, something is definitely wrong. Therefore, going to the doctor should only require a call. To confirm the diagnosis, your doctor may recommend additional tests.
A pelvic CT scan, pelvic ultrasound, an X-ray of the urinary tract, or magnetic resonance imaging (MRI) are all options.
Complications in pelvic organ prolapse
There can be complications due to this. But these are not life-threatening. Complications are primarily related to
- Pregnancy
- Fecal waste disposal
- Infection in the urinary bladder (because of obstruction in urination)
- Kidney problem, because of the problem in the bladder.
You should consult your doctor in such extreme cases.
Treatment Options For Urogynecology
How it is treated?
The issue can be addressed in a variety of ways. It also includes treatments and surgical procedures.
Treatments for behavior include mechanical and surgical procedures.
Non-Surgical treatment
It incorporates Social treatment and Mechanical Treatment. The first involves strengthening the pelvic muscles through exercises like the Kegel exercise. The second type, on the other hand, involves artificially supporting the organs. A pessary, for instance, is a support device that can be inserted into the vagina.
Surgical treatment
Obliterative surgery and reconstructive surgery are the two options for addressing this issue. The first is a significant choice. The vaginal opening that is meant to support the other pelvic organs is obliterated or gone.
The second method ensures organ reconstruction by repositioning the organs through an abdominal or vaginal incision. Reconstructive surgery covers a wide range of conditions. In one type, for instance, the organ’s prolapsed portion is attached to any pelvic ligament with the assistance of your tissues.
Sacrohystropexy is the second type. This is the route to take if you want to steer clear of having a hysterectomy. The best treatment for uterine prolapse is provided by this. The uterus is pushed upward after a surgical mesh is attached to the cervix.
The coporrhaphy is the third. It involves stitching the vagina so that both the front and back walls are strengthened.
Sacrocolpooexy is another name for it. This is done to treat the vaginal vault prolapse. Laparoscopy or surgical mesh attachment to the vaginal walls and the sacrum (tail bone) are the two methods used.
Expectations after surgery
After surgery, life should be easy. It will resolve pregnancy-related issues and other significant issues. The treatment is recommended by doctors as a long-term solution.
Restrictions following prolapse surgery and recovery Driving a lot of exercise The drip is taken out after 24 hours. Utilizing gauze can stop any bleeding that may occur in the vagina. Only when the bleeding stops is it taken out. Resting for a minimum of three to five weeks is recommended by doctors. From that point onward, you can have returned to an ordinary way of life.
Lifestyle changes after surgery
Constipation is common, so your main concern should be eating well. You ought to consume a lot of water. Fruits and vegetables, which are part of a healthy diet, can speed up your recovery.
Doing anything that puts pressure on your pelvis should be avoided. Laxatives and gentle exercises should only be used with your doctor’s approval.
Although the issue may appear to be significant, once you decide to address it, you will find a solution. You really want a positive outlook to battle such infections.
Urine Incontinence

What is Urinary Incontinence?
Urine incontinence is the urgent and frequent need for urination. The clinical meaning of urinary incontinence is the unintentional loss of pee. Due to the loss of control over the sphincters, it is primarily impossible to retain the urine. An overactive bladder is one of the major causes. Urinary dread is brought on by an involuntary contraction of the bladder wall muscle. One of the significant reasons for this issue is an overactive bladder. It has a psychological and social impact on people.
Everything You Need to Know About Urine Incontinence
There are six different kinds of incontinence in the urinary tract. Stress incontinence is a type of incontinence that occurs when an individual jumps, laughs, coughs, sneezes, or lifts something. Traumatic surgery, pregnancy, menopause, childbirth, and pelvic radiation are all potential causes of incontinence.
Urge incontinence is when a person experiences a sudden urge to urinate and loses a lot of urine. Urge incontinence can be brought on by pelvic trauma, pregnancy, menopause, childbirth, and certain neurological diseases like MS and Parkinson’s.
Blended incontinence
This mix is the consequence of inclination and stress incontinence. Mixed continence is caused by the same factors that lead to urge and stress incontinence.
Flood incontinence
Wasteful purging of the bladder brings about the continuous spillage of pee. The side effects of flood incontinence are much like that of stress incontinence. Multiple sclerosis, neurological damage, diabetes, spinal cord injury, or prostate enlargement are some of the causes of overflow incontinence.
This kind of urination loss is caused by problems with the urinary system. Cognitive and physical impairment, such as head injuries, immobility, and Alzheimer’s disease, are the root causes of functional incontinence.
Reflex incontinence
Spastic bladder or reflex incontinence happens when pee is filled in the bladder and a reflex that is compulsory makes the bladder agreement to discharge it. Injury to the T12 level of the spinal cord is one of the causes of reflex incontinence.
When to see a doctor?
If you are unable to control your urge to urinate, you should see a doctor right away. However, if you find that you need to use absorbent pads or change your underwear frequently, you should see a gynecologist for assistance.
Before it becomes embarrassing for you, you need to talk to your doctor. It is beneficial to seek medical attention because the problem with incontinence may result in:
Serious health problems Older adults are at greater risk because it can make them more likely to fall.
Your connections and social exercises would be restricted and now and then confined.
Symptoms of urinary incontinence
There are numerous side effects of urinary incontinence like:
- Spillage of pee during sniffling, strolling, hacking, or hopping.
- the strong desire to urinate and the uncontrollable loss of urine.
- when you suddenly change your position, which causes the urine to pass.
- When you reach orgasm, you will urinate.
- difficulties with passing urine.
- When you feel as though your bladder has not completely empty.
Causes of urinary incontinence
Urinary incontinence is not a disease. It is a symptom brought on by routines, persistent medical conditions, or a variety of physical problems. An intensive examination by the specialist can assist you with knowing the specific reason for the urinary incontinence.
Diuretics can be found in a variety of foods, drinks, and medications, which can lead to urinary incontinence. They invigorate the bladder and furthermore builds the volume of pee. Some diuretics include:
Caffeine, alcohol, chili peppers, chocolate, sparkling water, and carbonated beverages containing a lot of vitamin C, citrus fruits, sedatives, heart and blood pressure medications, and muscle relaxants
The incontinence may also be caused due to:
Clogging
The rectum and bladder share many nerves since they are near one another. The overactive nerves caused by the hard, compacted stool lead to an increase in urination frequency.
UTI or Urinary Plot Disease
The bladder becomes aggravated by the diseases that can make areas of strength for the pee.
Pregnancy The fetus’s increased weight and hormonal changes during pregnancy may cause incontinence.
Childbirth The bladder-controlling muscle may become weaker during a normal delivery. Additionally, it causes damage to the bladder’s nerves and supporting tissues. Prolapse results from this. Prolapse is when the uterus, bladder, rectum, and small intestine are pushed out of their normal positions and fall into the vagina, resulting in incontinence.
Aging The muscles in the bladder also get older, which makes it harder for the bladder to hold urine. Incontinence is caused by an increase in the involuntary bladder’s contractions as you get older.
Hysterectomy In women, numerous joint ligaments and muscles provide support for the uterus and bladder. The pelvic floor muscles are highly susceptible to injury during any surgery that affects a woman’s reproductive system. This could result in incontinence.
Estrogen is a hormone that helps the urethra and bladder stay healthy during menopause. There is less estrogen produced after menopause, which can cause tissue damage and eventually incontinence.
Incontinence as a result of enlarged prostate glands is the cause of a condition known as benign prostatic hyperplasia, which affects older men.
Prostate cancer Stress and urge to urinate can cause prostate cancer. A common side effect of treating prostate cancer is incontinence.
Stroke, multiple sclerosis, brain tumor, spinal cord injury, and Parkinson’s disease all have the potential to impair bladder control, which can lead to urinary incontinence.
Obstruction Tumors cause the normal flow of urine to be blocked, resulting in overflow incontinence. One common type of obstruction that results in urine leakage is urinary stones.
Treatment Options For Urogynecology
Diagnosis of urinary incontinence If you suffer from urinary incontinence, you must first visit a general practitioner. They are able to identify the kind of incontinence. When discussing your issues with a healthcare professional, do not be embarrassed.
A few questions will be asked by the general practitioner. Among them are:
What is the prevalence of urinary incontinence?
Whether it happens when you laugh or cough?
Do you have any issues when you urinate?
How much fluid, caffeine, or alcohol do you drink?
Are any medications being taken?
The general practitioner will also recommend some tests to determine whether or not you have incontinence. The general practitioner will first check the health of the urinary system. During your coughing or sneezing, a pelvic exam will be performed to check for any urine leakage.
Your vagina will likewise be inspected to affirm regardless of whether a piece of the bladder swells into the vagina, otherwise called a cystocele. It occurs in the event of stress incontinence.
The doctor will instruct you to place your fingers inside the vagina while compressing the pelvic floor muscle. If the pelvic floor muscle is damaged, urination will be difficult.
The general practitioner will first assess the health of the prostate gland in a male patient. The urethra is surrounded by the prostate gland, which is situated between the penis and the bladder. In order to feel the prostate gland, fingers must be inserted into the bottom during a digital rectal examination. Urinary incontinence will occur if the gland expands.
If the general practitioner believes that the symptoms are indicative of a UTI, or urinary tract infection, a dipstick test is performed on a sample of the patient’s urine. The presence of bacteria is determined by testing the urine.
The urine sample will be inserted into a chemical-testing stick. The presence of bacteria will be confirmed if the stick changes color. The little synthetically treated stick can likewise actually take a look at the presence of protein and blood in the pee.
The purpose of a residual urine test is to ascertain how much urine remains in the bladder after you urinate. This test is known as the leftover pee test. To determine how much urine is still in the bladder, an ultrasound scan is performed. It is for the most part estimated after a catheter depletes the bladder.
Different tests
The specialist will direct more assessments in the event that the reason for incontinence isn’t clear. The treatment for your concern will be begun first, and afterward further tests will be followed on the off chance that the continuous treatment shows no certain result.
Cystoscopy The cystoscopy procedure involves using a thin tube and a camera to get a better look at the bladder and the inside of the urinary tract. It helps to find any problems with the urinary tract or bladder that cause urinary incontinence.
Urodynamic tests are a group of tests that are done to check how the urethra or the bladder are working. You might be told to save a bladder journal for certain days and afterward go for different tests at the center or clinic. The tests include:
(I) Working out the bladder’s strain by inclusion of a catheter into the urethra
(ii) Working out the strain in the mid-region by addition of a catheter in the base
(iii) Estimating the stream and measure of your pee by requesting that you pee into a specific machine
Treatment for urinary incontinence
Treatment for urinary incontinence The kind of treatment you should use for urinary incontinence depends on the kind of incontinence you have and the symptoms you’re having. You will receive treatment for both urinary incontinence and any other medical conditions that may be contributing factors.
First, non-surgical and non-medical treatments are tried. Among them are:
Way of life changes
An overall doctor could recommend you go for a way of life change first to carry upgrades to your incontinence.
You might be advised to:
If you’re overweight, you should try to lose weight by: (i) cutting back on the amount of caffeine in your coffee, tea, or cola; (ii) drinking enough fluids each day; and (iii) avoiding caffeine-containing beverages altogether.
Training your bladder If you have urge incontinence, you will be told to train your bladder. In cases of mixed urinary incontinence, it can also be combined with muscle-building exercises for the pelvic floor. You will gain knowledge of a number of strategies that will eventually assist in extending the period of time between feeling the urge to urinate and passing urine. Six weeks will pass during this.
Training for the muscles of the pelvic floor The muscles of the pelvic floor control the flow of urine when you urinate. The urethra and bladder are surrounded by these muscles. Assuming the muscles of the pelvic floor are harmed or feeble, it can cause incontinence. You should frequently practice these muscles to keep away from incontinence.
It will be suggested that you start a program to learn how to exercise your pelvic floor muscles. The expert will evaluate your force of getting the pelvic floor muscles. Specific exercises will be given to you if you can contract your pelvic floor muscles. People who suffer from urinary incontinence are said to benefit from pelvic floor muscle training.
Medicines In the event that the above-mentioned treatment for stress incontinence does not result in improvement, surgery will be offered as the next option. Duloxetine, an antidepressant, will be given to you in the event that you are not a good candidate for surgery. The urethra’s muscle tone will improve as a result, ensuring that it stays close.
Duloxetine tablets will be given to you twice daily. Moreover, you want to go to the specialist following two to about a month. It is to determine whether the medication that was prescribed helped you or caused severe side effects.
If you have urge incontinence, your doctor will give you an antimuscarinic if the training for your pelvic floor muscles isn’t enough.
Risk factors
There are many gamble factors that lie with urinary incontinence. Among them are:
Age
The muscles of the urethra and the bladder debilitate as age increments. The chances of developing urinary incontinence rise as a result of the changes to the bladder, which tend to weaken it.
Gender Incontinence in the urn also varies by gender. Urinary incontinence affects the most pregnant, menopausal, and postpartum women with normal anatomy. Urinary incontinence, on the other hand, is most common in men with prostate issues.
Overweight If you are overweight, your bladder’s surrounding muscles feel more pressure. Because it weakens the bladder, when you cough or sneeze, urine leaks out.
Family Ancestry
The gamble of incontinence expansions on the off chance that any of the relatives have this issue. The greatest increase in risk is urge incontinence.
Smoking
In the event that you are dependent on tobacco, the dangers of getting urinary incontinence are a lot higher.
Complications
Numerous issues can arise from urinary incontinence. Among them are:
Infections You may increase your risk of contracting a urinary tract infection (UTI) as a result of incontinence. This risk is increased by the frequent urge to urinate.
Skin issues You may develop numerous rashes, skin infections, and sores as a result of incontinence. You are more likely to develop skin issues if you frequently get your skin wet.
Preventing urinary incontinence
Urinary incontinence can’t always be avoided, but there are ways to lower the risk:
- Try to do exercises that will help you strengthen your muscles in your pelvic floor.
- Do keep a legitimate weight.
- Try to quit smoking with professional assistance.
- Acidic food varieties, caffeine, and liquor aggravate the bladder. Do whatever it takes not to eat such food varieties.
- Fiber assists with forestalling stoppage. Attempt to consume more fiber.
Success rate of urological incontinence surgery
The success rate of urinary incontinence surgery ranges from 36% to 87%. The rate of success varies depending on the patient’s age and condition.
Cost of urinary incontinence surgery
The cost of surgery to treat urinary incontinence varies from Rs. 30,000 to Rs. 1,50,000. The range varies due to the possibility that some patients will require stress incontinence surgery while others will require urgent incontinence surgery.
Certain medications simply cannot always prevent urinary incontinence. However, in order to keep the problem from getting worse, you need to follow the advice of the doctor.
Pelvic Reconstruction

What is Pelvic Reconstruction?
Pelvic reproduction is one of the surgeries which assists with reestablishing the trustworthiness and strength of the pelvic floor. When the pelvic floor’s ligaments and muscles are damaged or weak, this procedure aids in treatment. This typically occurs during pregnancy. This is accomplished by treating each prolapsed organ and rebuilding the layers necessary to support or remove the fallen organ. Prolapse of the pelvic organs, chronic disease, heavy lifting, and surgery are all treated with this procedure.
Everything You Need to Know About Pelvic Reconstruction
How is a pelvic reconstruction done?
The technique of a pelvic remaking happens inside the vagina. An incorrectly placed incision along the mucosa (vaginal skin) that is overlying the bladder is used for an anterior pelvic reconstruction. Addition of the catheter is made into the urethra empowering the vaginal mucosa to open, and the bladder wall to uncover.
An anterior repair can be done in a variety of ways. An incision that runs along the front wall of the vagina, starting close to the entrance and finishing close to the top of the vagina, is one of the most common procedures. Specialists utilize absorbable join to fix the debilitated layers.
This surgery typically takes between 30 and 60 minutes to perform. It would take around 1 – 2 hours altogether in the event that a vaginal hysterectomy happens with pelvic recreation.
Pelvic reconstruction treatment
There are two treatment options for pelvic reconstruction. These are:
- The first non-surgical treatment that is frequently tried is a pessary. It is inserted into the vagina to control urine leakage and provide support for the pelvic organs.
Additionally, lifestyle and diet adjustments are suggested by doctors. A portion of the tips are:
Guarantee A legitimate measure of liquid admission.
Eat more foods that are fibrous. Include salads, green vegetables, or fruits.
Try to keep your BMI in a good range. Maintain your weight in check.
- Treatment with surgery Typically, surgical procedures are recommended if the issues have advanced. Depending on your medical condition and other clinical parameters, there are two types of surgeries performed.
(i) Obliterative surgery: This type of surgery makes the vagina smaller or wider. It assists with offering help to the prolapsed organs. After this strategy is finished, there will be zero chance of sex.
(ii) Reconstructive surgery Restoring the organs’ original positions is the goal of reconstructive surgery. This system is finished through an entry point in the vagina. The sorts of reconstructive medical procedure include:
Repair of native tissue.
Colporrhalphy is a treatment for prolapse of the vagina’s front and back walls.
Sacrocolpopexy is used to treat enterocele and prolapse of the vaginal vault.
Sacrohysteropexy is performed when a woman wants to treat uterine prolapse but does not want a hysterectomy.
Mesh is surgically implanted inside the vagina (it is used to treat all types of prolapse).
Treatment Options For Urogynecology
What to expect after surgery
Approximately six weeks after the surgery, expect some discharge and spotting from the vagina. Over time, bleeding goes down. On the off chance that draining increments, you want to quickly call your PCP. Dissolving stitches are exemplified by a yellowish-white and watery vaginal discharge.
Recovery time for pelvic reconstructive surgery
The circumstances and the patient’s condition determine the length of time the patient needs to recover from pelvic reconstructive surgery. Normally, it requires around three weeks after the medical procedure to get back to full action. After the surgery, the patient should not have any sexual contact for three to four weeks. This is because the patient would experience painful sexual activity if a vaginal incision was made. For the first few weeks, you should avoid lifting, vigorous exercise, and straining.
Cost of peThe expense of pelvic remaking goes from Rs. 3,50,000 to Rs, 5,55,000.
You need treatment right away if the symptoms of pelvic organ prolapse are hindering your daily activities. Specialists will propose non-careful choices first and, if necessary careful choices later on.
Cystoscopy

What is a Cystoscopy?
Cystoscopy is an interaction that permits a Urologist to review the underlining of the bladder and the urethra. It removes your urine from your body. The activity is carried out by the doctor using a cystoscope, a lens-enclosed hollow tube. He carefully moves the lens into your bladder after inserting it into your urethra. In most cases, the test is performed by the doctor in a room where the anesthetic jelly to numb your urethra is given to you. Cystoscopy can also be performed under general anesthesia. The way to deal with do Cystoscopy relies upon the reason for the issue.
Everything You Need to Know About Cystoscopy
Why is cystoscopy performed?
WCystoscopy aids in the identification, treatment, and monitoring of the primary cause of any issues you are experiencing with the bladder or urethra. In the event of the following, it is recommended that you go through the procedure:
Examine for signs like an overactive bladder, blood in the urine, and urine incontinence, or the inability to urinate even when trying, such as leaking or peeing every time. During urination, there may also be a sensation of pain in the bladder.
Finding the cause of frequent urinary infections is helpful. You don’t have to have a crystoscopy just because you have a urinary tract infection.
diagnosing conditions affecting the bladder, such as cancer, cystitis, inflammation, and stones.
It aids in the treatment of bladder diseases like small tumors or abnormal bladder tissues. The specialist involves extraordinary devices in a cystoscope to deal with a specific condition like a bladder growth.
It aids in the diagnosis of a enlarged prostate. A condition in which the urethra tube that goes through the prostate gland gets smaller is called an enlarged prostate. To determine whether it has narrowed or not, cytoscopy can be helpful.
When to get medical advice
When the conditions appear to be severe and you observe the following symptoms, you should seek medical attention.
Having abdominal pain and nausea; not being able to urinate after undergoing a cystoscopy; experiencing vivid red blood clots when peeing.
having a fever of more than 101.4 degrees Fahrenheit and experiencing a burning sensation when peeing for several days (over the past two days).
Preparing for a cystoscopy
You could need to take anti-microbials prior to going through Cystoscopy and after it on the off chance that you have a frail safe framework or a UTI. The specialist will gather your pee test before the test. For keeping a pee test, you should come without discharging your bladder toward the beginning of the day. Therefore, scheduling an appointment early in the morning is advised.
The doctor might give you general anesthesia for the test:
- So ensure you have somebody to bring you back home.
- Take a break when you get home before going to work.
- If you need to take any medications on a regular basis, ask your urologist. If you experience excessive bleeding, this medication can be used as a preventative measure.
Types of cystoscopy
There are two different kinds of cystoscopy: rigid cystoscopy and flexible cystoscopy. Both fill a similar need, yet the strategy contrasts a little.
Adaptable cystoscopy: The doctor performs the test with a cystoscope, a thin pencil-like instrument. This instrument bends easily. You remain awake throughout the procedure because you do not receive any anesthesia prior to it. It is not painful, but you may feel like you need to pee during the process, which is uncomfortable.
The cystoscopy procedure
Cystoscope rigid: Because the instrument is rigid, you are unable to bend it during a rigid cystoscopy. By administering anesthesia, the doctor can either completely unconscious you or numb only your lower extremities to carry out the procedure. When you get the injection, this process may hurt, but you won’t feel anything because you will be unconscious afterwards.
The cysBefore the procedure, you will first need to empty your bladder. Then, at that point, you should wear a medical clinic outfit and rests on the therapy bed. You can secure your feet to the stirrups for convenience. In case you get a bladder infection, the nurse will give you some antibiotics as a precaution.
You will receive anesthesia from the doctor; it tends to be any sort. However, if you score the general one, the testing will make you unconscious. You will remain awake if the doctor administers local or regional anesthesia, but the lower area will remain numb. In order to make the procedure less painful, the doctor uses a gel to dampen your urethra. Before inserting the cystoscope into the urethra, the doctor also coated it with gel. You may experience burning sensation and the desire to pee while inserting.
As the cystoscope enters the bladder, the specialist glances through the focal point to research it. Additionally, to facilitate the procedure, it secretes a sterile solution that fills the bladder. Due to this fluid, the doctor can easily see inside the urethra.
The test takes less than five minutes if the doctor uses local anesthetic. The procedure can take anywhere from fifteen to thirty minutes if he administers general anesthesia.
toscopy procedure
Risks of a cystoscopy
After undergoing a cystoscopy, there may be some risks. The stakes are as per the following:
- Even after two or three days, peeing still produces a burning sensation.
- It’s possible that you’ll urinate more often; at the point when this happens doesn’t control it as it might prompt a blood coagulation or blockage.
- During urination, you may experience bleeding.
- You might have a swollen urethra, which makes it hard to urinate. Consult your doctor if you are unable to urinate for more than eight hours.
- urinary tract infection. Fever, nausea, an excessive odor in the urine, lower back pain, and other symptoms of the disorder.
- Additionally, if you experience persistent stomach pain, see a doctor.
Treatment Options For Urogynecology
Complication of cystoscopy
The cystoscope can have the following effects:
Infection: Infections can occur in the urinary tract when cystoscopy is performed. In order to prevent infections like these, the doctors give you antibiotics before and after the test. The infectious urinary tract effect can be brought on by smoking, unique anatomy in the tract, and getting older.
Pain: Constant abdominal pain and burning sensation when urinating are the symptoms. These side effects are not all that extreme and decrease step by step after the test.
Bleeding: When you urinate, blood may come out, but it is not too much. In the event that there is extreme dying, counsel the specialist.
Recovering after a cystoscopy
There is some discomfort following the test, but it goes away over time. Nonetheless, don’t take headache medicine to decrease the aggravation as it can build the dying. You can ease the pain by doing the following:
Hold a clammy and comfortable fabric against the urethra opening to assist with facilitating the aggravation.
Take a nice, warm bath, but check with your doctor first because he or she might tell you not to.
After having a cystoscopy, drink a lot of water, about half a milliliter per hour. Do not delay after drinking water; whenever it is necessary, flush the bladder.
What to expect
During a Cystoscopy procedure
The doctor will either anesthetize you or sedate you before performing a cystoscopy. Depending on the type of anesthesia, it takes anywhere from fifteen to thirty minutes. The following procedure is followed by doctors:
Before the procedure, you must empty your bladder and lie down on the table.
Contingent on the sort of Cystoscopy you are going through, you could possibly get sedation or narcotic. The two sorts of medications go through your vein. On the off chance that you take a soothing, you will be completely mindful of the interaction. However, if anesthesia is used, you will remain unconscious throughout the procedure.
The doctor will then use anesthetic jelly to push the cystoscope into the urethra. The sedative jam keeps any aggravation from the addition. While larger cystoscopes collect the tissue sample, smaller scopes are more convenient to insert into the urethra.
After that, the doctor sterilizes the urethra without using any of the scope’s fluid. The doctor is able to conduct a more thorough examination of the urethra after this sterilization.
Using the scope’s lens, the doctor examines our urethra and bladder. The doctor might look inside the urethra with a special camera. The video is directly projected onto the screen by the lens.
After Cystoscopy Procedure
After Cystoscopy has been fruitful, you could get a few anti-toxins. Drinking alcohol should be avoided for at least 24 hours. Some of the process’s side effects include:
- In your urine, blood from urine may appear slightly pinkish or red.
- It could burn when you urinate on it.
- more frequently urinating.
What are the results of cystoscopy?
There are two possibilities: The physician will be able to discuss your issue or await the outcome right away. You will need to schedule a second appointment with your doctor to talk about the result if your doctor is waiting for it.
The doctor will send the cystoscopy sample to a laboratory for analysis if there is a case of bladder cancer. The doctor examines the reports for discussion following the research.
Cost of cystoscopy surgery
The surgery costs a different amount at each hospital. Yet, assuming that you have protection, you really want not stress over it. You can ask your urologist for a discount if you do not already have one.
In any case, in India, the medical procedure’s typical expense might go from 783 bucks to 4669 bucks, barring resection.
