What is Gynecologic Cancers?
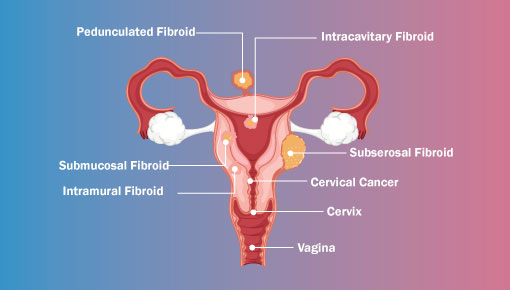
When it comes to reproductive organs in women, caution is vital. Cancer that develops in the reproductive organs of a woman is termed gynecological cancers. Doctors may find gynecological cancers in various places of a woman’s reproductive parts such as the cervix, ovary, uterus, etc.
You must keep track of your body so that you can immediately seek help from professionals when you experience any unusual changes in the body. Everyone may not have the same symptoms of gynecological cancers. Gynecological cancers are divided into six types, out of which three types are widespread, and the other three are very rarely seen.
Gynecologic cancers types
There are six types of gynecological cancers that are detected in women. Out of the six types of cancers, doctors find the three classes to be ubiquitous, and the rest are sporadic. Each type of cancer is unique and has its symptoms and signs.
Every woman is at risk of having gynecological cancers. The risk of getting affected by this cancer increases as the age increases. Treatment might prove to be effective if it is found at an early stage.
The six types of gynecological cancers are:
1. Uterine cancer
Women have a pear-shaped organ in the body known as the uterus. This is the area where the growth of the baby takes place. It is one of the most common types of cancer that is found in women. The chances of having this cancer increase with diabetes, obesity, and frequent estrogen use, especially without progesterone, and hypertension.
The sub-division of uterine cancers are endometrial stromal tumors, endometrial cancers, and uterine sarcomas. Doctors find endometrial cancer to be the most common type of cancer in the uterus.
If detected and diagnosed at a very early stage, endometrial cancer can be curable. It is treated by laparoscopic surgery, which is a minimally invasive surgery. The time taken for this surgery is a hospital stay of only 2-3 days. Some patients require post-surgery treatment. The post-surgery treatment requires either radiotherapy or a combination of chemotherapy and radiotherapy both.
2. Cervical cancer
This is another kind of gynecological cancer, which is also very common. Women in large numbers are affected by this kind of cancer all over the world. They often reach advanced stages because the awareness regarding this cancer is significantly less, and the screening facilities are also very poor. Human Papillomavirus or HPV infection is a common cause of cervical cancers.
Doctors suggest PAP tests or regular cancer screenings for detecting HPV. It may help to detect cervical cancer at an early stage. Early-stage detection helps to treat the tumor by radical surgery alone. If the cancer is detected at an advanced stage, it may require radiation and chemotherapy.
A very effective way to prevent this type of cancer is through the process of vaccination. This vaccination must be given before young girls are sexually active. The method of immunization is also useful in the case of other kinds of cervical cancers.
3. Ovarian cancer
Another most commonly detected gynecological cancer is ovarian cancer. The three kinds of ovarian cancer are stromal cell cancer, epithelial ovarian cancer, and germ cell cancer. Among all these cancers, epithelial cancer is the most common one. 85% of ovarian cancers are epithelial ovarian cancer.
Epithelial ovarian tumors that are benign in nature are cured by surgery, and the ones that are malignant are treated by chemotherapy or cytoreductive tumor surgery. An essential fact that you must know about epithelial ovarian cancers is that they can reoccur in advanced stages.
Younger individuals are found suffering from germ cell tumors, which is a form of ovarian cancer. 95% of the germ cell tumors are cured by surgery. Some of the cases require chemotherapy. Doctors often prefer fertility preservation therapy to treat young patients suffering from germ cell tumors.
Out of all the ovarian cancers, stromal cell cancer is the most slow-growing. This kind of cancer is treated with surgery.
4. Vulvar cancer
This is a sporadic form of gynecological cancer. The external genitalia of the female is mostly affected by vulvar cancer. It is very commonly detected in women who are elderly. This type of cancer is mostly curable. Doctors might perform radical surgery to treat vulvar cancer. Sometimes radiation therapy and chemotherapy are also needed.
5. Vaginal cancer
The other rare form of cancer is vaginal cancer. Women who are above the age of 50 years are mostly affected by this kind of cancer. In the case of vaginal cancer, Human Papillomavirus, or HPV injection, is responsible. Doctors perform radical surgery to treat vulvar cancer, and sometimes chemotherapy or radiotherapy is also needed.
6. Gestational trophoblastic tumor
GTD or gestational trophoblastic disease is a term given to a group of tumors that are related to pregnancy. These tumors are sporadic and subdivided into five more types. One of the classes is benign, and the other four types are malignant.
During the time of pregnancy, the tumors start growing in the layers of cells, which are known as trophoblast. Doctors use chemotherapy to treat these tumors. They are mostly curable.
When to see a doctor
There is no way by which you can be sure that you will be getting gynecological cancer. You need first to recognize the symptoms and signs of gynecological cancers before you seek any help. If you have abnormal bleeding from the vagina, talk to your doctor immediately. After menopause, any sort of vaginal bleeding needs treatment. You must ask for help from the doctors. If you have not reached the menopause stage but still notice you have heavier periods, which even lasts longer, or in case you are experiencing abnormal bleeding between your cycle, seek medical consultation. If you experience any of the symptoms or warnings that last for longer and are not usual, you must contact the doctor.
Gynecologic cancers causes
There are many causes of gynecological cancers. Some of the reasons are:
- Diabetes
- History of menstrual and reproductive problems includes having issues while conceiving or starting menstruation before the age of 12 and menopause after 55.
- Family history
- Smoking
- Older age
- Weak immune system
- HIV infection
- HPV infection
- Obesity
- High-fat diet
- Usage of fertility drugs or oral birth control drugs
- Any kind of prior radiation performed in the pelvic area
- Estrogen therapy
Gynecologic cancer symptoms
The symptoms of all gynecological cancers are not the same. Some of the symptoms might be similar, but not all. It mainly varies depending upon the individual, the kind of cancer, and its stage. In many cases, it is seen that some women may not even experience any such symptoms. Some of the symptoms of cervical cancer are:
- Pelvic area pain
- Abnormal bleeding from the vagina
- Discharge from the vagina is unusual
symptoms of endometrial cancer are:
- Pain during sex
- Pain during urination
- Abnormal bleeding from the vagina
- Pressure, pain, or lump in the lower belly
- Weight loss that is unexplained
symptoms of ovarian cancer are:
- Fatigue
- Constipation
- Diarrhea
- Loss of appetite
- Nausea
- Heartburn
- Indigestion
- Gas
- Discomfort in the abdomen
- Bleeding from the vagina
- Backache
- Weight loss that is unexplained
- Frequent urge to urinate
- Fluid buildup responsible for shortness of breath
symptoms of vaginal cancer are:
- Constipation
- A growth or lump
- Abnormal discharge
- Vaginal bleeding that is abnormal
- Pain sensation during urination
- Pain sensation during sex
- Pelvic pain which occurs frequently
- A feeling of burning or itching in the vulvar area
- A sore that is open and lasted for more than one month
- The white color of the skin on the vulva
- A rough sensation of the skin on the vulva
symptoms of uterine cancer are:
- Abnormal bleeding from the vagina
- Painful urination
- Difficulty while urinating
- Frequent urge for urination
- Feeling of pain during sex
- Pelvic pain that is frequent
symptoms of fallopian tube cancer are:
- Vaginal bleeding that is not usual
- Pelvic pressure or pain
- Mass or a lump found in the area of the pelvic
- Vaginal discharge that is not usual
Risk factors for gynecologic cancers
There are various risk factors for gynecological cancers. It all depends upon the age and the kind of cancer. Some of the risk factors are:
- Diabetes
- Obesity
- A weak immune system
- Smoking
- History of gynecologic cancer
Screening tests for gynecological cancers
The screening tests for gynecological cancers are:
- Colposcopy
- Cervicography
- HPV testing
- Polarprobe or Tuscan
- Ovarian carcinoma screening
- Biochemical markers
- CA125
- Genetic screening
- Proteomic technology
- Examination of the pelvic area
- Ultrasonography
Gynecologic cancer diagnosis
If you visit your gynecologist for regular checkups, it will assist in detecting gynecological cancers early. Your doctor will look for irregularities or unusual masses on the vulva, cervix, ovaries, uterus, and vagina during the pelvic exam. You will also go through a PAP test to check whether there is any presence of cells that are cancerous on the cervix or not.
If your gynecologist suspects any sign of cancer, specific diagnostic imaging tests will be performed, which includes:
- An ultrasound
- MRI or CT Scan
These tests will help the gynecologists to determine the extent of gynecological cancer. Doctors may also perform some additional methods to diagnose or screen gynecological cancer. Some of them are:
- Colposcopy
- D&C or Dilation and curettage
- LEEP or Loop Electrosurgical Excision Procedure
- Biopsy
- Laparoscopy
- HE4, CA-125, OVA 1 blood tests
Gynecologic cancer treatment
The treatments for gynecological cancers are done with advanced technology. During the process, doctors suggest compassionate care for women. The therapy will basically depend upon the extent of cancer, your overall health, and your strength of tolerance for different therapies you will undergo during the procedure. Some of the treatment options are:
- Surgery
Doctors prefer surgery as it is the primary treatment considered in the case of gynecological cancer. It helps remove the tumor, the organs that are affected, and the groin lymph nodes or the para-aortic lymph nodes. Gynecologic oncologists, who are specially trained using minimally invasive surgical instruments to remove the tumor. It helps in faster healing and also causes minimum pain.
- Radiation Therapy
Cancer cells are killed, and tumors are shrunk using radiation therapy. The radioactive waves help to conduct this procedure.
- Chemotherapy
The cancer cells are killed by consuming medicines orally or taking medications intravenously. These are popularly known as chemotherapy.
- Hormone therapy
This therapy focuses on stopping the growth of the cancer cells and kills them.
- Intraperitoneal chemotherapy
This chemotherapy involves administering directly into the cavity of the abdomen. This therapy is improving day by day, and patients are also improving for long-term survival.
- Clinical trials
Through these studies, researchers can find effective treatments that will help to cure gynecological cancers.
Gynecological cancers are curable when diagnosed at an early stage. It is a worldwide issue nowadays. Researchers are developing drugs that can deal with this cancer even at an advanced stage.
Cervical Cancer

What is Cervical Cancer?
At the point when malignant growth begins in the cervix, it is called cervical disease. Cervical cancer is a risk for every woman. Women over 30 are most likely to experience it. Dependable contamination with particular sorts of human papillomavirus (HPV) is the primary driver of cervical malignant growth. The HPV vaccine and screening procedures can aid in the prevention of cervical cancer. Girls between the ages of 9 and 45 may also benefit from receiving the HPV vaccine. Early detection of cervical cancer is associated with a long life expectancy and high quality of life, making it highly treatable.
Cervical cancer Signs & Symptoms
In most cases, early-stage cervical cancer does not cause any symptoms. In any case, during the high level phase of cervical disease, there are a few signs and side effects including:
After intercourse, vaginal dying
- Weighty vaginal release which has a foul scent
- Draining after menopause
- Torment during intercourse
- Pelvic agony
Cervical cancer causes
Cervical cancer develops when DNA mutations in healthy cervix cells begin to occur. The instructions that tell a cell what to do are carried by the DNA of the cell.
Healthy cells begin to grow and multiply at a predetermined rate and eventually die at a predetermined time. The changes illuminate the cells to develop and duplicate wildly, and they keep on living. A tumor is formed when abnormal cells multiply. Cancer cells can divide from a tumor and spread (metastasize) to other parts of the body by occupying nearby tissues.
There is no unmistakable view on what causes cervical disease, yet it is unequivocal that Human Papillomavirus (HPV) assumes a part in causing cervical malignant growth. The HPV virus is very common, and people who get it increase their risk of developing cancer. Your environment and lifestyle are also important factors in determining your risk of developing cervical cancer.
Types of cervical cancer
You can determine the course of a disease and the necessary treatment for two main types of cervical cancer:
Squamous cell carcinoma: This type of cervical cancer begins in the squamous cells, which are thin, flat cells that border the exocervix, the part of the cervix that extends into the vagina. Almost 90% of cervical diseases are squamous cell carcinomas.
Adenocarcinoma is a type of cervical cancer that begins in the column-shaped glandular cells that surround the cervical canal.
At times, the two kinds of cells engage in cervical disease. Rarely, cancer develops in the cervix’s other cells.
Cervical cancer risk factors
- Human papillomavirus (HPV) disease
- Having intercourse with different accomplices
- Smoking
- Conception prevention pills (oral contraceptives) utilized for quite a while
- Having brought forth at least three youngsters
- Engaging in early sexual contact
Complications of cervical cancer
- Early menopause: When your ovaries stop producing the hormones estrogen and progesterone, you enter menopause.
- The vagina becomes narrowed as a result of radiotherapy, which is used to treat cervical cancer. This makes sex painful or difficult.
- Lymphoedema: When your pelvic lymph nodes are removed, the lymphatic system’s normal operation is disrupted.
Screening test for cervical cancer
Cervical dysplasia affects more women in their 20s and 30s. Demise from cervical malignant growth is uncommon in ladies who are more youthful than 30 years and in ladies (of all ages) who have normal screenings alongside the Pap test. The Pap test is used to identify changes that can lead to cancer and cancer itself. As you get older, your risk of dying from cervical cancer goes up. As of late, passings from cervical disease are recognized a piece higher in people of color who are under 50 years than in white ladies who are under 50 years. Black women over the age of 60 are more likely than white women over the age of 60 to die from cervical cancer.
When a person does not present with symptoms, certain tests are used to screen them for various types of cancer. Studies demonstrate that screening for cervical cancer aids in lowering the disease’s death rate.
Tests for cervical cancer include:
Examine the pelvis twice: In this, the specialists really take a look at a lady’s body for any unusual changes in her cervix, uterus, vagina, ovaries, and other close by organs.
Pap exam: In this procedure, the doctor gently scrapes the vagina and cervix to obtain cell samples for testing.
HPV composing test: The Pap test is comparable to this test. The patient’s cervix-derived cell samples are examined.
A cervical cancer screening Pap test: After certain Pap test results, a HPV test is finished. a HPV test that can be done in conjunction with or without a Pap test to check for cervical cancer. for an HPV test, self-collected samples Clinical trials take cervical cancer screening tests one step further.
Cervical cancer stages
Stage 1: The cancer has only spread to the cervix, the womb’s neck, and has not grown into deeper tissues.
Stage 2: Cancer has spread beyond the uterus and cervix, but it has not reached the pelvic walls or the lower vaginal part. It hasn’t spread to the lymph nodes or other parts that are farther away.
Stage 3: Disease has spread to the lower portions of the vagina or the walls of the pelvis. However, cancer could be obstructing the ureters. It could have reached nearby lymph nodes or not.
Stage 4: Disease has spread to the bladder or rectum (back entry) or far off organs including the lungs or bones. It’s possible that cancer has also spread to lymph nodes and organs outside of the pelvis.
Treatment options by stage
Stage 1: The main treatment is surgery. Certain individuals likewise need chemoradiotherapy.
Stage 2: Chemotherapy and radiation therapy are the most common treatments. A patient may need to undergo a radical hysterectomy and radiation therapy in the worst cases.
Stage 3: Eventually, radiation therapy and chemotherapy are administered. After receiving internal radiation therapy, pelvic lymph node removal surgery may also be performed.
Stage 4: Chemo-radiotherapy is the main treatment. For approximately five weeks, external radiotherapy is administered on five consecutive days. At the end of the course, if necessary, a boost of brachytherapy is performed.
Cervical cancer prevention
Getting regular screenings to look for any cancerous cells can help prevent and treat cervical cancer. The HPV vaccine can also be beneficial.
This HPV vaccine was used to prevent HPV-caused cervical cancer in individuals aged 9 to 45. Infections caused by HPV16, HPV18, and five additional cancer-related HPV types can all be avoided with this vaccine.
Girls should get the HPV vaccine to help prevent cancer of the cervix. The best vaccination schedule can vary depending on a number of factors, including age and vaccine availability. Speak with a doctor about it.
There are additional steps people can take to help prevent cervical cancer, such as:
Use condoms and dental dams to have safe sex and limit the number of sexual partners they have. Avoid sexual intimacy with people who have had many partners. Avoid sexual intimacy with people who have genital warts or other symptoms. Quit smoking.
Cervical cancer during pregnancy
Survival rates for cervical cancer
Pregnancy and Early-Stage
Cervical Cancer If Your Doctor Finds Early-Stage Cervical Cancer, You Can Continue Your Pregnancy Safely After the birth, the treatment is delayed for several weeks; really at that time you will actually want to get therapy with a hysterectomy (evacuation of the uterus and cervix) or cone biopsy (expulsion of a piece of the cervix), in view of the movement of disease.
Treatment Options for Women with Advanced Cervical Cancer During pregnancy, treatment options become crucial for women with advanced cervical cancer. You and your doctor will talk about the possibilities. Assuming that serious cervical malignant growth is noticed, your pregnancy could get ended.
The chance to survive for at least five years after getting diagnosed with cervical cancer:
Stage 1 – 80-99%
Stage 2 – 60-90%
Stage 3 – 30-50%
Stage 4 – 20%
Cervical cancer treatment costs
Treatment for cervical cancer typically costs between $100,000 and $300,000 per month. In India, the cervical disease treatment modalities for example radiotherapy, brachytherapy, chemotherapy, and medical procedure, goes from Rs. 74000 to Rs. 222000.
Endometrial cancer

What is Endometrial Cancer?
The cells of the inner edging of the uterus are the source of endometrial cancer, also known as endometrial carcinoma. The most prevalent form of uterine cancer is this one. When cells in the endometrium—the inner lining of the uterus—start to grow out of control, endometrial cancer develops.
Cells in almost any piece of the body can become harmful and can spread to different pieces of the body. The most typical signs and symptoms of endometrial cancer are abnormal vaginal bleeding, spotting, or other discharge. Consult a doctor if you notice any of these CA endometrium symptoms.
Endometrial cancer symptoms
The symptoms of endometrial cancer are actually fairly straightforward to recognize. Therefore, bleeding is a common symptom in uterine cancer patients during menopause. When ladies go through menopause, which characterizes as no periods for one year, they shouldn’t have any further vaginal dying.
Therefore, any time you experience bleeding after menopause is abnormal and should prompt a gynecological examination.
Other symptoms include heavy bleeding during the period or a sudden change in the length of the menstrual cycle. Pain in the lower abdomen or the pelvis section are additional potential symptoms of uterine cancer. Whether you have sex or not, you can feel pain.
When to see a doctor
It is in your best interest to contact the best gynecologist whenever you experience any of these symptoms. You should get checked out even though these symptoms are not a sign of a serious condition.
A doctor will help you pinpoint the exact issue and suggest the best course of treatment for the disease.
Endometrial cancer causes
Endometrial cancer is difficult to diagnose in the majority of cases. Specialists say that adjustments of progesterone and estrogen in the body assume a urgent part in uterine malignant growth. The endometrium may be impacted if the sex hormone shifts.
Fortunately, endometrial cancer is discovered in its early stages in the majority of women who present with the condition. This is because women frequently experience abnormal uterine bleeding. The majority of endometrial cancers occur in women who have stopped having periods for a long time after menopause.
Then, all of a sudden, there will be bleeding. Any draining after menopause, whether it be simply blood strain or critical stream, should be assessed, and it should be upset to demonstrate that it isn’t disease in the uterine coating.
Types of endometrial cancer
Let’s now examine the various kinds of endometrial cancer. The majority of uterine cancer cases are adenocarcinomas, according to the American Cancer Society’s report. From the glandular tissue, it emerged.
Squamous cell, small cell, uterine carcinosarcoma, and serous carcinoma are the most common types of uterine cancer. Uterine cancer comes in a variety of forms and can be divided into two categories.
Type 1: The cancer tissue in type 1 grows slowly and does not spread quickly to other parts of the body.
Type 2: The cancer cells in this type are more active, and they rapidly and aggressively spread outside the uterus.
Endometrial cancer risk factors
Obesity is one of the risk factors for uterine cancer. Obese women have a six-fold higher risk of developing endometrial cancer than women of average weight.
There are a number of explanations for this increased risk of endometrial cancer. Endometrial cancer is more likely to occur in women with elevated circulating estrogen levels and prolonged estrogen influence.
Endometrial cancer during pregnancy
Pregnancy-related cancer is uncommon, but it can happen. Fortunately, since cancer rarely directly affects the baby, pregnant women with cancer can deliver healthy babies. Cancer treatment during pregnancy, on the other hand, is extremely difficult.
Therefore, pregnant women with cancer must be treated by a skilled medical team. During all stages of pregnancy, surgery is regarded as the most secure method of treatment. It makes a little gamble the developing child.
During the second and third trimesters, think about chemotherapy as a protected decision. The placenta fabricates fencing around the child, which impedes a few sorts of chemotherapy medications to go through. This leaves the child unaffected. However, the baby may still be harmed indirectly by some forms of chemotherapy.
Anemia and malnutrition, two side effects that affect the mother, pose a threat to the unborn child. Drugs used in chemotherapy also have the potential to induce premature labor and low birth weight. Because of the risk of birth defects or miscarriage, chemotherapy use during the first trimester is typically discouraged.
Complications of endometrial cancer
Abnormal vaginal bleeding is endometrial cancer’s most common complication. Other than that, bleeding from the vagina after menopause. You may also experience lower abdominal pain or pain during or after sexual activity. It is preferable to see the best gynecologist if you are experiencing pain or irregular periods. After conducting the necessary tests, they will determine the issue and provide you with the most effective treatment.
Tests to diagnose endometrial cancer
- Make an appointment with the gynecologist right away if you notice any of the symptoms associated with endometrial cancer. The first step is for the doctor to inquire about the issue and review your medical history. Endometrial biopsy, hysteroscopy, dilation, and curettage (D&C), and other necessary tests will be recommended to you.
- During an endometrial biopsy, a doctor inserts a thin, flexible tube into your uterus to diagnose your cervix. Through the line, they will remove a small amount of tissue from the endometrium.
- A flexible tube equipped with a camera will be inserted into the uterus during the Hysteroscopy test. They will use this to collect abnormality samples and conduct a visual examination of the issue.
- The last test that will assist with diagnosing endometrial malignant growth is Enlargement and Curettage (D&C). On the off chance that the biopsy result isn’t precise or incapable to comprehend, they will encourage you to do Expansion and Curettage (D&C). The cervix is dilated during this procedure, and a special tool is used to remove tissue from the uterus. In the wake of gathering the example, they will send the example to the research facility. The professional will correctly test the model there, and the report will be sent to the doctor. After that, a doctor will know what the problem is and start treating you accordingly.
Endometrial cancer staging and treatment options
Endometrial cancer is discovered very early, as mentioned in the beginning. The cancer cell will spread slowly from the uterus to other parts of your body even if you don’t feel any symptoms. There are four stages of cancer, according to scientists. To learn the four steps, read the section below.
Stage 1: The cancer is only present in the uterus during the initial stage.
Stage 2: In the second stage, the cancer cell began to spread and began attacking your cervix.
Stage 3: The cancer cell has now spread outside of the uterus and fallopian tube at this stage. During this stage, it can also attack the vagina and ovaries. The majority of patients can be cured through local radiation therapy and surgery.
Stage 4: This is the last stage. Cancer thus spreads beyond the pelvis and uterus. The cancer cell spreads to the kidney, bladder, and other organs. The person in stage 4 meets with the doctor on a regular basis. Chemotherapy and radiation are the main treatments for patients in phase 4. Patients with cancer in its advanced stages, or stage 4, require chemotherapy, radiation therapy, and surgery all at once.
Endometrial cancer prevention
You can lower your risk of developing uterine cancer by using home remedies. The following section explains some treatments:
Weight management: The issue typically affects people who are overweight or obese, as was mentioned earlier. You must lose weight in order to stop endometrial cancer cells from spreading. You ought to follow a singular eating regimen outline and admission good food and vegetables.
Get Moving Everyday: A solid and in great shape body can oppose endometrial disease. In order to get in shape, you should exercise freehand for at least an hour. It has additional advantages.
If you notice abnormal vaginal bleeding, seek assistance: At the point when you track down strange draining from the vagina or extreme agony, quickly talk with the specialist. They will direct you in the most effective manner.
Really take a look at the Benefit and Impediments of Chemical Treatment: Always contact the physician. Consult your doctor if you are considering hormone therapy. They will do things better than you because they have years of experience.
Do not conceal anything from the physician: You will always receive the best guidance from the best physician. Therefore, tell them everything you know. Describe the issue in detail. Also, let people know if your family has Lynch syndrome in the past. After that, the doctor might tell you to get the tests you need.
Endometrial cancer survival rate
The disease is typically discovered in its early stages; subsequently, it tends to be restored. Consequently the endurance rate for a particular stage is 90 %. Endometrial cancer can only be cured by maintaining a healthy weight, getting some exercise on a regular basis, and consulting with a doctor. The outlook for the long term will be improved by each treatment and diagnosis.
Endometrial cancer treatment costs
The cost of treating endometrial cancer cannot be mentioned. You must spend less than those in phase 4 if you are in stage 1.
Vulvar Cancer

What is Vulvar Cancer?
Vulvar cancer is a type of cancer that affects the female genital organs’ outer surface. The clitoris, the labia majora and minora, and the opening of the vagina make up the vulva, which is the outer part of the female genitals. Vulvar cancer can occur at any age, but most cases are found in older people.
Vulvar cancer symptoms
The symptoms of vulvar cancer are:
- burning sensation and persistent itching on the vulva
- vulva thickening and changes in color, such as a color that is redder or whiter than usual, in the vulva’s skin texture.
- ulcers or swollen bumps on the vulva that persist.
- Bleeding that is not menstrual.
Vulvar cancer causes
It is still unclear what exactly causes vulvar cancer. Most of the time, doctors know that a cell develops cancer when its DNA begins to change (mutations). A cell’s actions are determined by its DNA. The mutations instruct the cell to rapidly divide and grow. The dead cells are replaced by the living cell and its offspring. The accumulated cells form tumors that have the potential to become cancerous, occupy nearby tissues, and spread throughout the body.
Vulvar cancer types
Doctors plan the most effective treatment of Vulvar Cancer depending on the type of cell in which cancer begins. The most common types of vulvar cancer are:
- Squamous cell carcinoma of the vulva is a type of cancer that affects the vulva’s inner and outer folds. Around 90% of vulvar malignant growths are squamous cell carcinomas.
- Adenocarcinoma is a type of cancer that typically begins in the Bartholin glands, which are located inside the vaginal opening and produce mucus to lubricate the vagina. Adenocarcinoma accounts for about 8% of vulvar cancers. It incorporates melanoma as well as basal cell carcinomas and sarcomas.
Vulvar cancer risk factors
Despite the fact that the specific reason for vulvar malignant growth isn’t known, there are sure factors that can expand the gamble of the illness, including:
Age: Although vulvar cancer can happen at any age, the risk goes up as you get older. The typical age at diagnosis is 65.
Exposure to the human papillomavirus (HPV): HPV is an infection that spreads through sexual contact and is responsible for a variety of cancers, including vulvar and cervical cancer. HPV is spread to a lot of young people who are sexually active. The infection changes the cells and raises the risk of cancer in the future, but it sometimes goes away on its own.
Smoking: Another factor that contributes to an increased risk of vulvar cancer is smoking.
In order to undergo an organ transplant, some people take medications that suppress the immune system, which increases their risk of vulvar cancer. On the other hand, people who have conditions that weaken the immune system, such as HIV, are more likely to get vulvar cancer.
Skin condition including the vulva – White spot sickness (Lichen sclerosis), causes the slight, white patches in the genital region, builds the gamble of vulvar disease.
Tests to diagnose vulvar cancer
- X-beam of the chest – A x-beam of the chest is to be finished to check whether disease has spread to your lungs.
- A computerized tomography (CT) scan is a series of x-ray images taken all over your body from various angles. A CT scan is usually not necessary, but it can be recommended for women to look for large vulvar tumors or enlarged lymph nodes. Additionally, they are helpful in determining whether a sentinel lymph node procedure to check groin lymph nodes for cancer spread should be performed.
- Scanners for magnetic resonance imaging (MRI) make use of radio waves and powerful magnetic fields to produce images of the body’s organs. It is used to look for enlarged lymph nodes in the groin and pelvic tumors. Patients with early vulvar disease, as a rule needn’t bother with this test.
- Positron Emission Tomography (PET) scan: A radioactive drug is used in a PET scan to show where cells are more active than usual in your body. The organs of the body are depicted in three dimensions during this test. This test helps identify cancer cells and determine whether lymph nodes have been affected by the disease.
- In most cases, a PET-CT machine, which combines a CT scanner with a PET scanner, is used to learn more about cancer’s localization and spread.
Vulvar cancer symptoms
The symptoms of vulvar cancer are:
- Burning sensation and itching on the vulva that does not go away.
- Changes in the texture of the skin of the vulva, such as the color can be redder or whiter than usual and thickening of the vulva.
- Swelled bumps or ulcers on the vulva that does not go away.
- Non-menstruation bleeding.
Vulvar cancer causes
It is still unclear what exactly causes vulvar cancer. Most of the time, doctors know that a cell develops cancer when its DNA begins to change (mutations). A cell’s actions are determined by its DNA. The mutations instruct the cell to rapidly divide and grow. The dead cells are replaced by the living cell and its offspring. The accumulated cells form tumors that have the potential to become cancerous, occupy nearby tissues, and spread throughout the body.
Vulvar cancer types
Doctors plan the most effective treatment of Vulvar Cancer depending on the type of cell in which cancer begins. The most common types of vulvar cancer are:
- Vulvar squamous cell carcinoma – This type of cancer is found on the inner and outer folds of the vulva. About 90% of vulvar cancers are squamous cell carcinomas.
- Adenocarcinoma – This type of cancer usually starts in the Bartholin glands (found inside the entrance of the vagina and secretes mucus to lubricate the vagina). About 8% of vulvar cancers are adenocarcinoma. It also includes melanoma as well as basal cell carcinomas and sarcomas.
Vulvar cancer risk factors
Even though the exact cause of vulvar cancer isn’t known, there are certain factors that can increase the risk of the disease, including:
- Age – Though vulvar cancer can occur at any age, the risk increases with age. The average age for diagnosis is 65 years.
- Exposure to human papillomavirus (HPV) – HPV is an infection that spreads by sexual contract resulting in various cancers, including vulvar cancer and cervical cancer. A lot of young, sexually active people are exposed to HPV, in which the infection causes a change in cells and increases the risk of cancer in the future but in some cases, the infection goes away on its own.
- Smoking – Smoking is another reason for an increase in the risk of vulvar cancer.
- Weak immune system– To undergo an organ transplant, sometimes peopletake medications to suppress the immune system, which increases their risk of vulvar cancer while there are people suffering from conditions that weaken the immune system, such as human immunodeficiency virus (HIV), have an increased risk of vulvar cancer.
- Skin condition involving the vulva – White spot disease (Lichen sclerosis), causes the thin, white patches in the genital area, increases the risk of vulvar cancer.
Tests to diagnose vulvar cancer
- X-ray of the chest –An x-ray of the chest is to be done to see if cancer has spread to your lungs.
- Computerized tomography (CT) scan – A CT scan is a series of x-ray images taken from different angles around your body. Usually, a CT scan is not needed but can be suggested for women to detect large vulvar tumors or enlarged lymph nodes. They are also helpful in deciding whether a sentinel lymph node procedure should be done to check groin lymph nodes for cancer spread.
- Magnetic Resonance Imaging (MRI) – MRI scanners use strong magnetic fields and radio waves to generate images of the organs in the body. It is used to examine pelvic tumors and to identify enlarged lymph nodes in the groin. Patients with early vulvar cancer, usually don’t need this test.
- Positron Emission Tomography (PET) scan – PET scan uses a radioactive drug to show the areas of your body where cells are more active than normal. This test creates 3D images of the internal body organs. This test helps to spot the cancer cells and see if cancer has spread to lymph nodes.
Usually, a machine combined with a PET scanner and a CT scanner (called a PET-CT) is used, to get more information about areas of cancer and cancer spread.
Treatment Options For Gynecologic Cancers
Vulvar cancer stages
Doctors determine the stage of cancer by examining the tumor and the cancer’s spread to lymph nodes and other organs. The tumor’s size is expressed in centimeters (cm).
Stage 1: The cancer has not spread, consequently it is just in the vulva or the vulva and perineum.
1 (A): The tumor is no larger than 2 centimeters and no deeper than 1 millimeter.
1 (B): The tumor is deeper than 1 millimeter and larger than 2 cm.
Stage 2: The tumor is any size and has spread to nearby areas, such as the lower part of the urethra, vagina, or anus. It has not yet reached any lymph nodes or other organs.
Stage 3: The cancer has spread to the groin lymph nodes and nearby tissues like the vagina, anus, and urethra. There is no distant metastasis.
3 (A): There are either one or two metastases to lymph nodes that are smaller than 5 millimeters, or there is one metastasis that is 5 millimeters long.
3 (B): There are at least three metastases to lymph nodes that are less than 5 mm in size, or there are at least two metastases that are 5 mm in size.
3 (C): The cancer has spread to nearby tissue, one or more lymph nodes, and the lymph node capsule, or covering, around them.
Stage 4: Cancer has spread to a distant part of the body, the upper vaginal or urethral region, or both.
4 (A): Cancer has either attached the lymph node to the tissue below it or spread to regional lymph nodes, resulting in ulceration.
4 (B): Malignant growth has spread to a far off piece of the body.
Treatment options by stage
Stage 1
Treatment options depend on the size, depth, and presence or absence of a Ventral Intermediate Nucleus (VIN) in the patient. It can be surgically removed with a 1 cm edge of normal tissue around it if the depth is less than 1 mm (stage IA) and no other area is affected by cancer or VIN.
A partial vulvectomy and inguinal lymph node dissection (removal of nearby groin lymph nodes) are two options for stage IB cancer treatment. Sentinel lymph node biopsy can be used in place of lymph node dissection. If there is evidence of cancer in the lymph nodes, chemotherapy and radiation are administered.
A complete radical vulvectomy and removal of the groin lymph nodes are performed for larger and more extensive cancers.
On the off chance that the patient isn’t sufficiently solid to get the medical procedure, the lymph hubs are not eliminated, rather, radiation treatment can be given to the crotch regions. If the lymph nodes are enlarged, they can be examined with a needle biopsy prior to treatment to determine whether or not they contain cancer cells.
Stage 2
When the cancer is in stage II and has spread to structures near the vulva (the anus, the lower vagina, and/or the lower urethra), partial radical vulvectomy may be an option for treatment. Surgery, also known as sentinel node biopsies, involves removing the lymph nodes in the groin on both sides of the body. If cancer cells were removed from the edges of the tissue during surgery, radiation therapy can also be administered following surgery.
Radiation (regardless of chemotherapy) can be utilized as the primary therapy for ladies who are sick or powerless because of other clinical issues.
Stage 3
In stage III, when cancer spreads to nearby lymph nodes, surgery to remove cancer and groin lymph nodes (radical wide local incision or partial or complete radical vulvectomy) is required. In addition, radiation therapy may be administered after it. Once in a while chemotherapy (chemo) is likewise given alongside the radiation to work all the more successfully.
Cancer can also be treated with radiation (with or without chemotherapy) first, followed by surgery to remove any remaining cancer, in order to preserve normal structures like the urethra, anus, and vagina.
For patients who can’t go through a medical procedure because of other clinical issues, radiation and chemo (without medical procedure) can be utilized as the principal therapy.
Stage 4(A)
In stage IV (A), malignant growth spreads to a greater extent to organs and tissues in the pelvis (like the rectum (over the butt), the bladder, the pelvic bone, the upper piece of the vagina, and the upper piece of the urethra). The goal of surgery is to get rid of as much cancer as possible. The cancer-containing organ decides whether or not the surgery should be extended. Another option is pelvic expulsion, but it is rarely used.
A common treatment involves chemo, radiation, and surgery all at once. Surgery can precede or follow radiation therapy. Surgery can also be preceded by chemotherapy.
Radiation and possibly chemotherapy may be administered to women who are unable to undergo surgery due to other medical conditions.
Treatment with radical vulvectomy and the removal of the groin lymph nodes is an option if the tumors have spread to nearby lymph nodes but not to nearby organs. In this case, the lymph nodes have become ulcerated (open sores) or stuck to the underlying tissue. Surgery can be performed either before or after radiation therapy—usually combined with chemotherapy.
Stage 4(B)
There is no standard therapy for disease that spread to lymph hubs in the pelvis or organs and tissues outside the pelvis. Although surgery won’t likely cure these cancers, it can help relieve symptoms like blocked bowels or bladders. Chemotherapy and radiation can reduce cancer and alleviate symptoms.
Vulvar cancer during pregnancy
Pregnancy vulvar cancer The main treatment for vulvar cancer is surgery, which can be done during pregnancy or in the postpartum period (the time immediately following delivery). Before 36 weeks of pregnancy, local excision or vulvectomy (with or without lymphadenectomy) are the most common surgical procedures.
vulvar cancer survival rate
86% of people with stage 1 vulvar cancer survive for at least five years after receiving their diagnosis. However, the five-year survival rate for vulvar cancer drops to approximately 16% once it reaches its advanced stage and is classified as stage 4.
Vulvar cancer treatment costs
The cost of treating vulvar cancer in India varies depending on the stage of the disease and the hospital. As a result, vulvar cancer treatment costs can range anywhere from Rs. 258415 to Rs. 885900 INR (approximately $3500 to $12,000 USD).
With the development of new technologies, there are now numerous options that can assist in the fight against vulvar cancer. You should be aware of the disease’s symptoms so that it can be detected early and treated quickly.
Ovarian Cancer

What is Ovarian Cancer?
Disease that occurs because of the strange development of qualities that controls cell development change is known as ovarian malignant growth. The female regenerative framework contains two ovaries, one on each side of the uterus. The eggs (ova) and the sex hormones estrogen and progesterone are produced by each ovary, which is about the size of an almond. Female characteristics like breast development, body shape, and body hair are largely influenced by these hormones.
Symptoms for ovarian cancer
The most common symptoms women are likely to have if the disease has spread, but is at an early-stage ovarian cancer include:
- Bloating
- Pelvic or abdominal (belly) pain
- Trouble eating or feeling full too soon
Urinary side effects like inclination tension or torment in the bladder and regular pee.
Non-cancerous diseases or cancers of other organs also frequently cause these symptoms. At the point when the referenced side effects are caused because of ovarian disease, they will generally go on for quite a while and change from typical − for example, they happen all the more much of the time or are more extraordinary. The majority of these symptoms are experienced by women who do not have ovarian cancer and are caused by other conditions. However, if you experience these symptoms more than 12 times per month, see a doctor to determine the cause and, if necessary, receive treatment.
The following are additional signs of ovarian cancer:
- Fatigue (extreme tiredness)
- Constipation
- Upset stomach
- Abdominal (belly) swelling with weight loss
- Back pain
- Pain during sexual intimacy
- Changes in a woman’s menstrual, such as heavy or irregular bleeding
Causes of ovarian cancer
Gene mutations that you inherit from your parents account for some cases of ovarian cancer. BRCA 1 and BRCA 2 are the genes known to increase ovarian cancer risk.
Recently, it was discovered that cells at the back end of the fallopian tubes, rather than necessarily in the ovary itself, are the source of ovarian cancer. Ovarian cancer may be caused by male hormones (androgens), according to another theory.
Types of ovarian cancer
The ovaries have three main types of cells, hence, a tumor can develop in any of them. The three types are:
- Epithelial cells, which cover the surface of the ovary
- Germ cells, which make eggs (ova)
- Stromal cells, which hold the structure of the ovary together and make the hormones estrogen and progesterone.
Epithelial Tumors
A tumor begins in the layer of tissue that covers the ovaries in the majority of cases of ovarian cancer. It occurs frequently in women who have gone through menopause.
It does not necessarily mean that you have cancer if the doctor finds an epithelial tumor. The majority of epithelial tumors are not cancerous. Serous adenomas, mucinous adenomas, and Brenner tumors are examples of these benign epithelial tumors.
A carcinoma is the name given to the epithelial tumor if it is cancerous. It is additionally separated into various subtypes in view of the perception made under a magnifying lens. These are the four types of carcinoma:
- Serous (the most common subtype)
- Mucinous
- Endometrioid
- Clear Cell
A carcinoma is undifferentiated if the tumor cells do not match any of these subtypes. This means that they tend to grow and spread more quickly than the other four subtypes of a tumor.
To classify an epithelial tumor as cancer, it must sometimes be clearly visible. It is known as borderline epithelial ovarian cancer or a tumor with low malignant potential (LMP). Because it does not grow as quickly or spread in the same way as other types of epithelial cancer, this is not as dangerous to life.
Germ Cell Tumors
Ladies in their 20s are ordinarily impacted by these cancers. Regardless, they are available to women of any age. Most growths that start in microorganism cells are harmless.
Germ cell carcinomas have few subtypes, and tumors can also be a combination of multiple subtypes. These are the four main subtypes:
Teratoma shows up as the three layers of a creating undeveloped organism when inspected under a magnifying lens. A mature teratoma is the benign variant. Teratomas of infancy are malignant, or cancerous. This type of tumor is extremely uncommon and typically affects girls under the age of 18.
Although it is still extremely uncommon, dysgerminoma is the most prevalent form of germ cell cancer. This kind of cancer does not spread or grow more quickly. Most ladies who get this malignant growth are in their young or 20s.
Endodermal sinus tumor, also known as yolk sac tumor, is most common in children under the age of one, but it can develop at any time in a person’s life.
Choriocarcinoma develops and spreads quickly, happens in a lady’s belly. They rarely occur.
Ovarian Stromal Tumors
The diagnosis of these tumors occurs earlier than that of others. Granulosa-theca tumors and Sertoli-Leydig cell tumors are the most prevalent subtypes. Rare are both. Granulosa cell tumor (GCT), a rare subtype, is also present.
Treatment Options For Gynecologic Cancers
Ovarian cancer risk factors
Following are the ovarian cancer risk factors:
Age: The likelihood of developing ovarian cancer rises with age. After menopause, most ovarian cancers develop.
Obesity or excess weight: Ovarian cancer has been linked by studies, though not necessarily to all types that pose a threat to life.
Ovarian cancer can be increased by having a child after the age of 35 or by never having a child.
Treatment for Infertility – Although there has been conflicting evidence, some studies demonstrate a link between IVF (in vitro fertilization) treatment and borderline ovarian tumors.
Hormone Therapy: This involves receiving hormone therapy for a long time after menopause, particularly estrogen alone (without progesterone).
Family Ancestry – Having a family background of ovarian, bosom, or colorectal disease can build the gamble.
Having Had Bosom Disease – The characteristic changes raise malignant growth risk for both bosom and ovarian tumors.
Smoking: Although it rarely raises overall risk for ovarian cancer, smoking is linked to an increase in a rare epithelial ovarian cancer tumor known as a mucinous carcinoma.
Complications of ovarian cancer
- Infection
The treatment that is being used to treat this disease sometimes kills healthy cells, like white blood cells. The body is shielded from germs and bacteria by white blood cells. Therefore, a lower white blood cell count increases the likelihood of infection.
- Bleeding and Bruising
Advanced ovarian cancer treatments can damage the platelets that help to stop bleeding. With fewer platelets, one can experience bleeding longer than usual and develop larger and continual bruises.
- Loss of Fertility and Menopause
To treat cancer, women may have to have a portion of their reproductive system taken out. Assuming that the specialist eliminates both the ovaries as well as your uterus, you will not be able to become pregnant. Additionally, in the event that the ovaries are eliminated, you should go through menopause (in the event that you have not recently gone through it).
- Neuropathy
Some chemotherapy drugs, result to cause nerve harm or neuropathy. While the issue deteriorates, you can encounter deadness, shivering, and torment in your furthest points.
- Hearing Loss
Chemotherapy drugs can also damage the nerves that lead to the ear. This can affect your hearing or cause ototoxicity.
- Other Complications
The individuals who are going through ovarian disease treatment can likewise encounter inconveniences like weakness, queasiness, retching, balding, loss of hunger, mouth wounds, rashes on all fours, bone diminishing, and skin changes (stripping and rankling).
Tests to diagnose ovarian cancer
Pelvic ultrasound:
An ultrasound takes a picture of the internal organs by using sound waves. Using a wand, this can be done internally or on top of your skin (abdomen). A transvaginal ultrasound is an internal ultrasound that does not require any preparation and is painless. During the test, the doctor checks the ovaries for any changes like an increase in size or growths.
Other imaging tests that aid in ovarian cancer diagnosis include:
MRI (magnetic resonance imaging).
- CT scan (computed tomography).
- PET scan (positron emission tomography).
- Chest X-ray
Blood tests:CA-125 is the substance that is examined through blood tests. Elevated degrees of this substance in the blood is shown as an indication of malignant growth. Even if cancer is present, CA-125 levels are frequently normal, whereas many conditions that are not cancer-related have higher levels. Therefore, blood tests are finished with different tests to analyze ovarian disease.
Surgical evaluation: During surgery, it is possible to diagnose ovarian cancer. Operation and chemotherapy are also used to treat ovarian cancer.
Laparoscopy: A laparoscope, a thin camera, is inserted through a small abdominal cut in this type of surgery. The doctor evaluates cancer, performs staging biopsies, and, in some cases, removes ovarian tumors using the scope and ports that hold instruments.
Stages of ovarian cancer
Stage 1
In this stage, cancer is only in the ovaries.
Stage 1A: Only one ovary is affected by cancer.
Stage 1B: Only one ovary is affected by cancer.
Stage 1C: Both ovaries are affected by cancer. Additionally, one of the following has occurred during Stage 1C-1. Cancer cells have entered your belly or pelvis as a result of surgery.
Stages 1 to 2 Before surgery, either cancer of one of the ovaries or a tumor filled with fluid has burst, releasing cancer cells into the abdomen.
Stage 1C-3.Cancer cells are tracked down in the liquid from the mid-region or pelvis.
Stage 2
At this point, the cancer has spread to the organs near the ovaries. It hasn’t spread to your organs in other parts of your body or to your lymph nodes.
- Stage 2A: Your cancer has spread to the fallopian tubes, uterus, or both.
- Stage 2B. Malignant growth has spread to organs in the pelvis like the bladder, colon, or rectum.
Stage 3
In this stage, disease has spread to local organs like the uterus and bladder. Additionally, cancer has spread to the lining of the stomach, the lymph nodes behind the belly, or both.
(A) Disease is in the close by lymph hubs and will in general fill in neighboring organs.
Malignant growth in the lymph hubs is under 10 mm.
Larger than 10 mm cancer in the lymph nodes
- ( B) Small malignant growth stores are in the stomach lining, and must be seen with a magnifying lens. Malignant growth can likewise be in neighboring lymph hubs.
- 2. During surgery, cancer is found in the belly, but it is less than 2 cm in size. They can likewise be outside your liver and spleen and in the lymph hubs.
- The growth of cancer is greater than 2 cm.
Stage 4
The cancer has spread to some distant organs at this most advanced stage.
- Although cancer cells are present in the fluid surrounding the lungs, the disease has not spread outside of your abdomen or pelvis.
- Cancer is found in the tissues and organs as well as in the lymph nodes. This might incorporate your skin, lungs, or mind.
Treatment options by stage
Surgery to remove the tumor is the primary treatment for stage 1. The doctor may sometimes recommend that the fallopian tubes or nearby lymph nodes be removed.
The treatment for stage 2 includes bilateral salpingo-oophorectomy and hysterectomy. The specialist will attempt to eliminate however much as a cancer as could reasonably be expected. Chemotherapy is recommended for at least six cycles following surgery.
For stage 3, treatment is a medical procedure and chemotherapy.
Chemotherapy and surgery are two of the treatment options for stage 4.
Ovarian cancer prevention
Ovarian cancer can’t be prevented, but the following things can lower the risk of developing the disease.
- taking contraceptives for at least five years.
- Had a tubal ligation (getting the cylinders tied), ovaries eliminated, and a hysterectomy (a medical procedure wherein the uterus, and in some cases the cervix, is taken out).
- after giving birth.
- Ovarian cancer risk can be modestly reduced by breastfeeding for at least a year.
Ovarian cancer during pregnancy
The majority of ovarian tumors discovered during pregnancy are not cancerous, and the ones that are typically cancerous are typically in their early stages. This indicates that the infant’s life is not in danger. In addition, moderate surgery that removes just the affected ovary and fallopian tube can help a lot of women keep their fertility. If cancer is discovered in its early stages (stages 1 and 2), fertility can often be managed. It is possible to perform a unilateral salpingo-oophorectomy, leaving the ovary and fallopian tube on the opposite side, in order to preserve fertility, if the ovarian cancer is discovered before metastasis.
Survival rates for ovarian cancer
All types of ovarian cancer have a 5-year survival rate of 45%. Individuals analyzed before age 65 have a higher endurance rate. Those who are diagnosed with stage 1 ovarian cancer or early-stage ovarian cancer have a 92% 5-year survival rate.
Ovarian cancer treatment costs
Ovarian cancer treatment is typically covered by health insurance; however, certain medications and treatments may not be covered by some plans. Ovarian cancer treatment can cost as much as $200,000 for advanced-stage cancer, which includes both surgery and chemotherapy, for patients who do not have health insurance.
Breast Cancer

What is Breast Cancer?
In basic terms, Bosom Disease is a sickness where the bosom cells develop wildly. It occurs when malignant (cancerous) cells grow in the breast, according to medical terms. In addition, these breast cancer cells spread to other parts of the body when they reach full size. Metastasis starts in the lymphatic framework which assists with shipping lymph (a liquid containing disease battling white platelets) and other safe framework cells all through the body, to battle malignant growth. The flawless metastasized malignant growth cells, travel through the lymphatic vessels and get comfortable far off body areas, consequently, frames new cancers, and keep the sickness cycle in presence.
Symptoms for breast cancer
Some common symptoms of breast cancer are:
- Lump formation in the breast
- Changes in skin, such as swelling, irritation, or itchiness
- Change in the shape and size of the breasts
- Pain and tenderness, even if no lump is felt
- Changes in the color and temperature of the breast
- Effects on the nipple, like
- Retraction (pulls inward)
- Dimpling or peeling
- Pain in the nipple area
- Redness
- Sore in the nipple
- Nipple discharge other than breast milk
When to see a doctor
If you notice any changes or lumps in your breast, see a doctor. The early signs of breast cancer can be detected with the help of a mammogram.
Main Causes Of Breasts Cancer
Breast cancer is caused by cells growing out of control. As a result, breast cancer is the result of abnormal changes and mutations in genes that control healthy cell growth. The most regularly known are bosom malignant growth quality 1 (BRCA 1) and bosom disease quality 2 (BRCA 2), which can expand the gamble of bosom disease.
The abnormal cells divide and continue to multiply, resulting in a mass or lump. Cells travel through your breast to your lymph nodes or other body parts.
Commonly, bosom disease begins with cells in the pipes (obtrusive ductal carcinoma). It can likewise start in the glandular tissue known as lobules (obtrusive lobular carcinoma), or in different cells or tissue inside the bosom.
The researchers have identified environmental, hormonal, and lifestyle factors that can raise the risk of breast cancer. Yet, the justification for why certain individuals with risk factors foster disease, yet others with risk factors never do, isn’t known. There is probably a complicated link between the environment and the genotype that causes breast cancer.
Breast cancer types
Different types of breast cancer are classified according to the affected cells found in the breast.
1) Non-invasive breast cancers: The majority of breast cancers are carcinomas, which are tumors that start in the epithelial skin tissue or organ-covering tissue. Adenocarcinoma, which develops in milk-producing glands or milk ducts, is the most common type of breast cancer.
2) Invasive breast cancers: The majority of breast cancers are invasive (also known as infiltrating). It can spread to healthy breast-circumference tissues. The most typical are:
Treatment Options For Gynecologic
Invasive ductal carcinoma (IDC) is a type of cancer that begins in the milk duct and spreads outside the duct into the breast’s fatty or fibrous tissue. It accounts for approximately 80% of all breast cancer diagnoses and is the most prevalent type.
Obtrusive lobular carcinoma (ILC) – This disease starts in the milk-delivering organs (lobules) of the bosom. The lymph nodes and other areas may also be affected by this. It addresses around 10 to 15% of all obtrusive bosom malignant growth.
There are some more uncommon yet serious bosom malignant growths, which are created in various ways, which influence their treatment methodology.
3) Triple-negative breast cancer (TNBC): This type of cancer is characterized by the absence of estrogen or progesterone receptors in the cancer cells. It is responsible for between 10% and 15% of all cases of breast cancer. The malignant growth cells don’t construct a very remarkable protein called HER2.
4) Inflammatory breast cancer (IBC) causes the breasts to become swollen, red, and tender. As a result, lymphatic vessels in the breast skin are obstructed by the cells. It represents around 1% to 5% of all bosom malignant growths.
Paget’s disease of the nipple is a rare form of breast cancer that affects the skin of the nipple and the areola, or dark circle, around the nipple. These changes resemble eczema. Because of its rarity, it only accounts for about 1-3% of all breast cancer cases.
Phyllodes tumors are another uncommon form of breast cancer. Because they develop in the connective tissue of the breast rather than the ducts, they are a type of sarcoma. A subsequent pathologist is expected to get the affirmation as this disease is the most extraordinary.
Angiosarcoma: Breast sarcomas are uncommon and account for less than one percent of all breast cancers. Cells that line blood vessels or lymph vessels become angiosarcoma. It can appear as a bruise-like lesion that grows over time and affects the skin. After receiving breast radiation treatment, the likelihood of it occurring is approximately 8-10 years.
Cancers
Breast cancer risk factors
Factors that are related to an increased risk of breast cancer include:
Gender: Women are more likely than men to develop breast cancer.
Expanding age-As your age builds, your gamble of bosom malignant growth increments as well.
Breast cancer history: If you have breast cancer in one breast, you are more likely to develop cancer in the other breast as well.
Family ancestry In the event that your mom or sister were determined to have bosom disease, particularly early on, your gamble of bosom malignant growth increments.
Exposure to radiation: You are more likely to develop breast cancer if you have ever had chest radiation treatments as a child or young adult.
Obesity: Being overweight raises your breast cancer risk.
The monthly cycle started at a more youthful age – In the event that your period began before age 12, your gamble of bosom disease increments.
Starting menopause at a later age: Starting menopause after the age of 55 increases the risk of developing breast cancer.
Having your first child later in life: Women who have their first child after the age of 30 may be more likely to develop breast cancer.
Alcohol consumption: Consuming alcohol raises one’s risk of developing breast cancer.
Complications of breast cancer
Though breast cancer surgery is safe, there can be several complications.
Psychological complications are:
- Fear
- Stress
- Insomnia (trouble falling asleep)
- Low sexual desire
- Depression due to physical changes appearing from the intensive treatments
Secondary physical issues are:
- Inflammation of lung tissue
- Heart failure
- Secondary Cancer can develop
Complications that can occur after the surgery are:
A hematoma is a blood clot outside of a blood vessel; a seroma is a buildup of clear fluid in a tissue, organ, or body cavity; chemotherapy-caused hair loss; nausea and vomiting; constipation or diarrhea.
Tests to diagnose breast cancer
If any symptom is discovered, the doctor will suggest several tests, such as:
Mammograms are breast x-rays that aid in the detection of any abnormalities.
Bosom Ultrasound – Checking the consequences of a mammogram is utilized. An ultrasound determines whether the breast lump is a solid tumor or a cyst filled with fluid.
Biopsies: During this procedure, tissue from the suspicious area is taken out and examined under a microscope for signs of breast cancer.
Imaging by magnetic resonance (MRI): This is utilized to track down the size of bosom malignant growth. Large magnets and radio frequencies are used in an MRI procedure to locate some small breast lesions missed by mammography. Multiple images of breast tissue are taken with it.
Stages of breast cancer
Stage 1– Stage 1 is divided into two stages as 1(A) and 1(B)
1A Stage: The tumor is up to 2 centimeters in size, but there is no involvement of the lymph node.
1B Stage: The growth size is under 2 centimeters, however there are a little gathering of disease cells, close by lymph hubs. It is also included in this stage if there is no tumor but a small group of cells nearby lymph nodes.
Stage 2 – Stage 2 is divided into two stages as 2(A) and 2(B).
2A Stage: can be used for any combination of the following:
There is no tumor, but there are one to three lymph nodes near the breastbone or under the arm.
Cancer of the lymph nodes under the arm and tumors up to 2 centimeters in size are both conditions.
The lymph node is not involved, and the size of the tumor is between 2 and 5 centimeters.
B Stage: can be used for one of the following:
The size of the tumor ranges from 2 to 5 centimeters, and there is a small group of cancer in one to three nearby lymph nodes.
The size of the tumor is greater than 5 centimeters, but there is no involvement in the lymph node.
Stage 3 – Stage 3 is divided into three stages 3(A), 3(B), and 3(C).
3A Stage: either of the following is assigned:
Malignant growth in 4 to 9 close by the lymph hubs, regardless of a cancer.
Growth size is bigger than 5 centimeters, in addition to a little gathering of disease cells in lymph hubs.
B Stage: The tumor has spread to the chest wall, and it may also have:
gotten into or through the skin.
Spread up to 9 lymph hubs under the arm region or close to the breastbone.
C Stage: It’s possible that there is no tumor in the breast; however, if there is one, it may have spread to the breast skin or the chest wall.
10 or more lymph nodes in the underarm
Lymph hubs close to the collarbone.
Lymph nodes located close to the breastbone and under the arm.
Stage 4 –
Cancer has reached stage 4 and has spread to distant organs. As a result, it is referred to as metastatic breast cancer or advanced breast cancer. Cancer may be present in the lungs, brain, liver, or bones at this stage.
Breast cancer treatment options by stage
The primary treatment for breast cancer in stage 1 is surgery. If doctors are able to remove all of the tumors along with a lining of healthy tissue around them and still leave enough tissue for the breast to look the same as before the surgery, then breast-conserving surgery is recommended.
In the active treatment of breast cancer, stage 2 requires three to eighteen months or more. It could be as simple as surgery and six weeks of radiation, or it could include chemo, radiation, and biologic therapies all rolled into one.
In stage 3, medical procedure, known as a mastectomy is alluded to eliminate harmful tissue alongside the lymph hubs. Damage to cancerous cells or tumors can also be caused by radiation therapy. Stage 3 cancer is frequently treated with chemotherapy.
Stage 4 is treated primarily with systemic medications. A few normal therapies like a medical procedure, radiation treatment, or territorial chemotherapy are likewise utilized. It is critical to address the emotional wellness gives that a phase 4breast malignant growth conclusion might cause.
Breast cancer preventions
Some of the preventions of breast cancer are:
- Maintain a healthy weight
- Do exercise regularly
- Stop drinking alcohol, or limit alcohol consumption
- Consult the doctor before taking birth control pills
- Do breastfeed your children, if your breast produces milk
- Eat healthy foods such as whole grains, fruits and vegetables, fish, eggs, and meat
Breast cancer during pregnancy
It is feasible to be recognized with bosom malignant growth during pregnancy, in any case, it is uncommon and isn’t caused because of the pregnancy. When a woman is diagnosed with breast cancer while she is pregnant, she feels a lot of anxiety because she is worried about the child’s safety. Despite the distressing and difficult circumstances, there is still hope for both mother and child thanks to the numerous treatment options.
Breast cancer survival rates
The endurance rate for bosom malignant growth is a lot higher when contrasted with some other tumors. The following are some survival rates:
- Breast cancer has a 5-year survival rate of 90%.
- Breast cancer has a 10-year survival rate of 84%.
- The 15-year endurance pace of bosom disease is 80%.
Breast cancer treatment costs
Breast cancer treatment is typically covered by health insurance if the patient has it; however, some plans may not cover specific medications or treatments. In the event that the patient doesn’t have medical coverage, bosom disease therapy essentially costs $15,000 to $50,000 or something else for a mastectomy or $17,000 to $35,000 or something else for a lumpectomy followed by radiation.
Try not to be stressed over bosom malignant growth. The endurance paces of bosom malignant growth are great yet it should be analyzed at a beginning phase.
